Original
Changes in the Pattern of Use of the Emergency Departments in an Spanish Oversaturated Tertiary Hospital Complex During COVID-19 Pandemic
Cambios en el patrón de uso de los servicios de urgencias en un complejo hospitalario terciario español sobresaturado durante la pandemia de COVID-19
Actual Med.2022;107(815):27-33 DOI: 10.15568/am.2022.815.or03
Recibido: 28/06/2021
Revisado: 15/01/2022
Aceptado: 02/03/2022
Abstract
Background and objectives: To analyze the effects of COVID-19 in the pattern of use (number of admissions, hospitalizations, hospitalization ratio, and classification by priorities) of Emergency Departments (EDs) of one tertiary referral hospital.
Methods: Retrospective, observational and single-center study, carried on in the EDs of Virgen de las Nieves Hospital Complex (Granada, Spain). The information was collected from the three hospitals which belong to the Virgen de las Nieves Hospital complex (i.e. the General Hospital, GH; the Children’s Hospital, CH; and the Neuro-Trauma Hospital, NTH) from February 1st to July 31st, 2019, and 2020.
Results: In the period under analysis, there were 71236 admissions compared with 118382 in the same period in 2019, which means an overall reduction of 38.83%. Considering the hospitalizations, there were 6841 compared with 7648 (2020 and 2019, respectively) which gives an overall reduction of 10.55%. The distribution of the priorities did not show a defined pattern; while CH and NTH’s EDs showed clear changes in their distribution, no notable changes were observed in GH’s ED.
Conclusion: The Covid-19 Pandemic changed dramatically the pattern of ED referral in our tertiary referral hospital. A noticeable reduction of admissions and hospitalizations were reported, together with a pronounced increase in the hospitalization ratio that in some cases reached almost 50%. This could be explaining for many reasons, such as the fear of contagion and the lockdown that presumably caused a decrease in the less-severe cases attended. Possibly, the effects of COVID-19 may have been indirectly influenced by the health care system of each country. The COVID-19 pandemic constitutes one of the greatest challenges in modern medicine, understanding better these changes and the impact that COVID-19 has caused on pattern of use of EDs will probably lead us to manage and use better our public health systems in the future.
Keywords: Emergency departments; COVID; Coronavirus; Admission pattern; Spain
Resumen
Antecedentes y objetivos: Analizar los efectos de la COVID-19 en el patrón de uso (número de pacientes atendidos en urgencias, hospitalizaciones, ratio de hospitalización y clasificación por prioridades) de los Servicios de Urgencias (SU) de un hospital terciario de referencia.
Métodos: Estudio retrospectivo, observacional y monocéntrico, realizado en los SU del Complejo Hospitalario Virgen de las Nieves (Granada, España). La información se recogió en los tres hospitales que pertenecen al Complejo Hospitalario Virgen de las Nieves (es decir, el Hospital General, GH; el Hospital Infantil, CH; y el Hospital Neurotraumatológico, NTH) desde el 1 de febrero hasta el 31 de julio de 2019 y 2020.
Resultados: En el periodo analizado se produjeron 71236 atenciones en urgencias frente a 118382 en el mismo periodo de 2019, lo que supone una reducción global del 38,83%. Considerando las hospitalizaciones, hubo 6841 frente a 7648 (2020 y 2019, respectivamente) lo que da una reducción global del 10,55%. La distribución de las prioridades no mostró un patrón definido; mientras que los SU de CH y NTH mostraron cambios claros en su distribución, no se observaron cambios notables en el SU de GH.
Conclusión: La pandemia de Covid-19 cambió drásticamente el patrón de derivación a urgencias en nuestro hospital terciario de referencia. Se constató una notable reducción de los pacientes atendidos en urgencias y las hospitalizaciones, junto con un pronunciado aumento de ratio de hospitalización que en algunos casos alcanzó casi el 50%. Esto podría explicarse por muchas razones, como el miedo al contagio y el bloqueo que presumiblemente provocó una disminución de los casos menos graves atendidos. Posiblemente, los efectos de COVID-19 pueden haber sido influenciados indirectamente por el sistema sanitario de cada país. La pandemia de COVID-19 constituye uno de los mayores retos de la medicina moderna, entender mejor estos cambios y el impacto que COVID-19 ha causado en el patrón de uso de los servicios de urgencias probablemente nos llevará a gestionar y utilizar mejor nuestros sistemas de salud pública en el futuro
Palabras clave: Urgencias; COVID; Coronavirus; Patrón de ingreso; España.
Leer Artículo Completo
1. INTRODUCTION
The sudden outbreak of coronavirus disease in December 2019 (COVID-19) has been a major issue to global health. To date, there are more than 132 million infected people and more than 2.8 million deaths reported worldwide, with the USA as the most affected country. Spain, with more than 3 million infected and 76.000 deaths, has been one of the most stressed countries in Europe. The Spanish National Health System (SNHS) was critically overwhelmed during the first wave of the pandemic in March, April, and May 2020 (1).
WHO declared COVID-19 as a pandemic on March 12th, 2020. Two days later, the Spanish government declared the “State of Alarm” and confined the population. After that, the de-escalation process happened in four phases with minimum differences between regions. Granada is a medium-sized city in the south of Spain, where two main hospitals cover a population of almost 900 000 inhabitants. In the city of Granada, the peak of the pandemic came a little later than in the rest of the neighboring cities.
Most of the hospital departments have changed their protocols adapting to the new situation during the COVID-19 pandemic, using telemedicine (2,3,45) as one of the main ways for delivering medical care, while keeping the usual assistance to the emergency cases. Therefore, the Emergency Departments (EDs) have been opened as usual with minimal changes, consisting mainly of special protocols and differentiated circuits for patients with suspected COVID (6). There was also a general call by the government and health care authorities warning the population not to attend the hospital unless needed during the lockdown.
The way that the COVID-19 Pandemic has affected the number of admissions, hospitalizations, hospitalization ratio, and classification by priorities in EDs is uncertain. Thus, we carried out a detailed analysis about the different pattern of use of the EDs in the only tertiary referral hospital in Granada, Spain (Virgen de las Nieves Hospital Complex) during the COVID-19 Pandemic, from February 1st to July 31st 2020, and compared to the same period in 2019. Possibly, a larger knowledge of these parameters would allow us to better manage a future COVID outbreak.
2. MATERIALS AND METHODS
2.1 Study Design
This is a retrospective, observational and single-center study, carried out in the EDs of Virgen de las Nieves Hospital Complex (Granada, Spain), which covers a population of near 500000 inhabitants. The information was collected from the Electronic Medical Records of the three centers that form the complex: General Hospital (GH), Children’s Hospital (CH), and Neuro-Trauma Hospital (NTH). The period for data collection included from February 1st to July 31st (2019 and 2020,181 and 182 days respectively).
2.2 Description of collected variables
The collected variables were the number of admissions, number of hospitalizations, and classification by priorities; no personal data from patients was collected.
The following concepts were defined: 1) Hospitalizations: patients who needed to be hospitalized for inpatient care; 2) Admissions: patients attending the ED who did not need to be hospitalized and were discharged in ED for home care; 3) Hospitalization ratio: the division between the number of hospitalizations and admissions.
The classification of patients was divided into five priorities according to the Manchester Triage System (MTS). The MTS is a priority classification system for patients in the EDs and it is widely used in Europe. This system classifies the patients into five colors, indicating the urgency levels and the ideal timing for delivering the first medical care: red (immediate, emergency; priority 1), orange (within 10 minutes, very urgent; priority 2), yellow (within 60 minutes, urgent; priority 3), green (within 2 hours, standard; priority 4) and blue (within 4 hours, non-urgent; priority 5) (7,8).
3. RESULTS
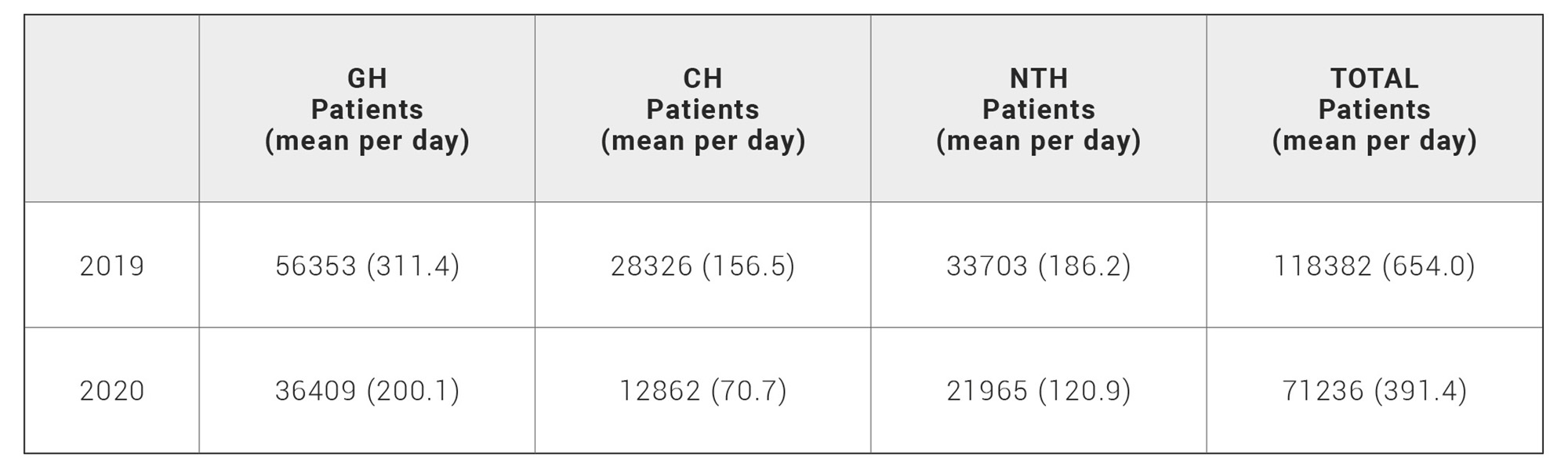
Differences in the number of admitted patients in the 3 centers comparing the same dates of 2019 and 2020 were found. Globally, the EDs of the Virgen de las Nieves complex admitted 118382 patients between the February 1st and the July 31st in 2019, and 71236 patients during the same period of 2020; this difference represents a 38.83% of overall reduction in the number of admissions. Reduction in each complex was 35.39%, 54.59%, and 34.83% (GH, CH and NTH; respectively) (Table 1).
Table 1. Patients admissions in Virgen de las Nieves Hospital Complex in the period covered.
GH, General Hospital; CH, Children’s Hospital; NTH, Neuro-Trauma Hospital
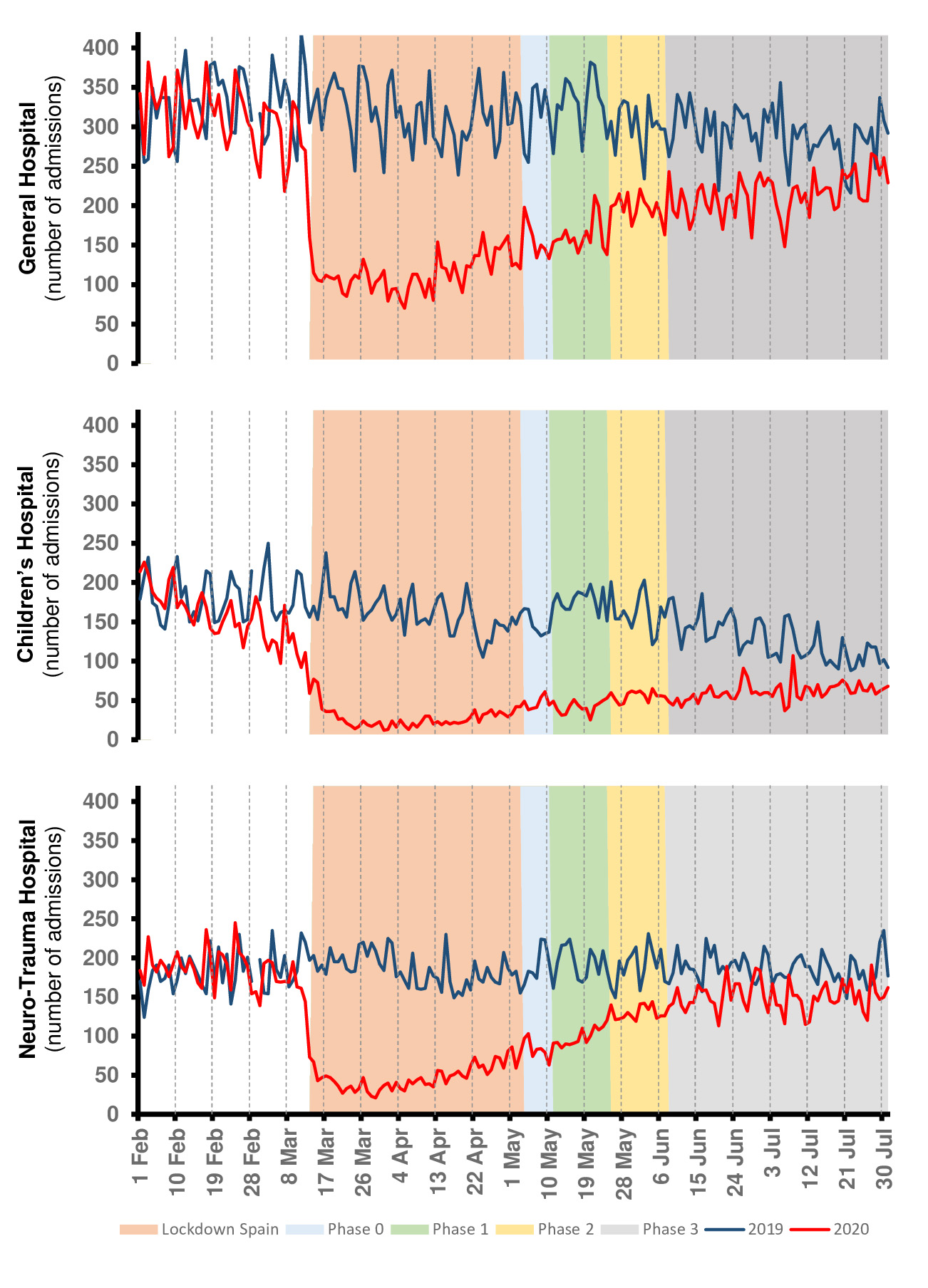
The evolution of EDs admissions in the different centers of the Hospital Complex followed a clear pattern that is shown in Fig 1. There was a marked decrease in the number of patients who came to these EDs coinciding with the beginning of the lockdown. The curve shows a slow increase in the numbers as the lockdown progressed, but still clearly different from the past year. Surroundings phase 3 of the de-scalation process, the pattern is very similar compared to 2019.
Figure 1. Emergency Departments admissions in the General Hospital, the Children’s Hospital and Neuro-Trauma Hospital of Virgen de las Nieves Hospital Complex.GH, General Hospital; CH, Children’s Hospital; NTH, Neuro-Trauma Hospital
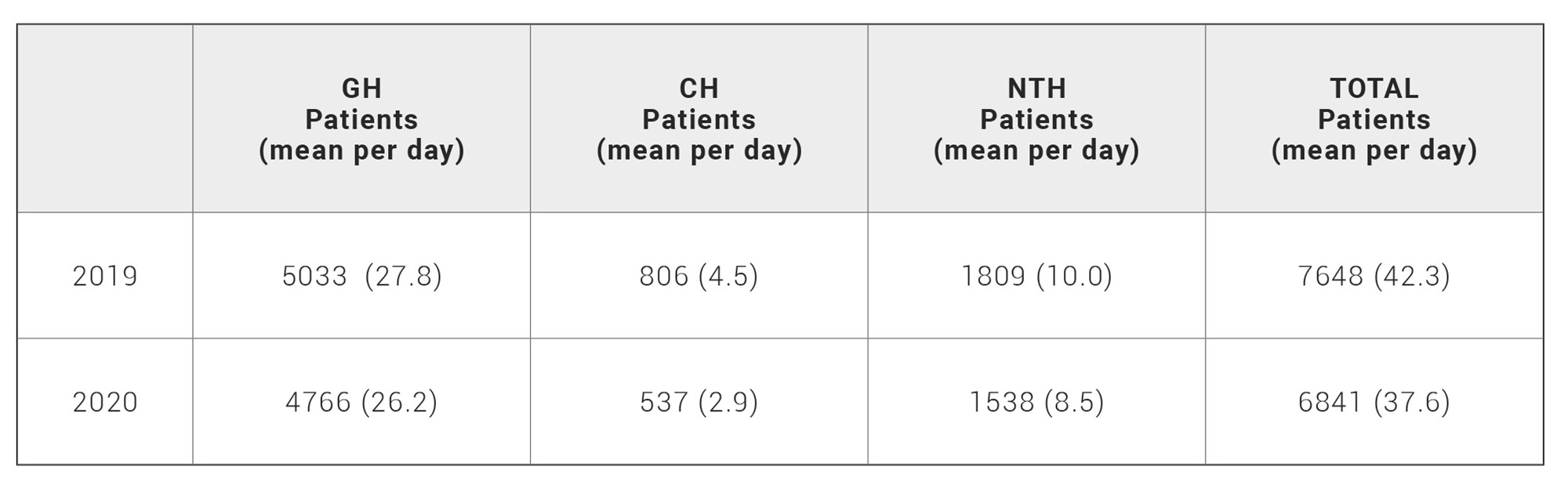
Regarding hospitalizations, from February 1st to July 31st 2020, there were 6841 compared with 7648 in the same period in 2019, which gives an overall reduction of 10.55%. Decrease in hospitalizations in each complex was 5.30%, 33.37%, and 14.98% (GH, CH and NTH; respectively) (Table 2).
Table 2. Patients hospitalization in Virgen de las Nieves Hospital Complex in the period covered.
GH, General Hospital; CH, Children’s Hospital; NTH, Neuro-Trauma Hospital
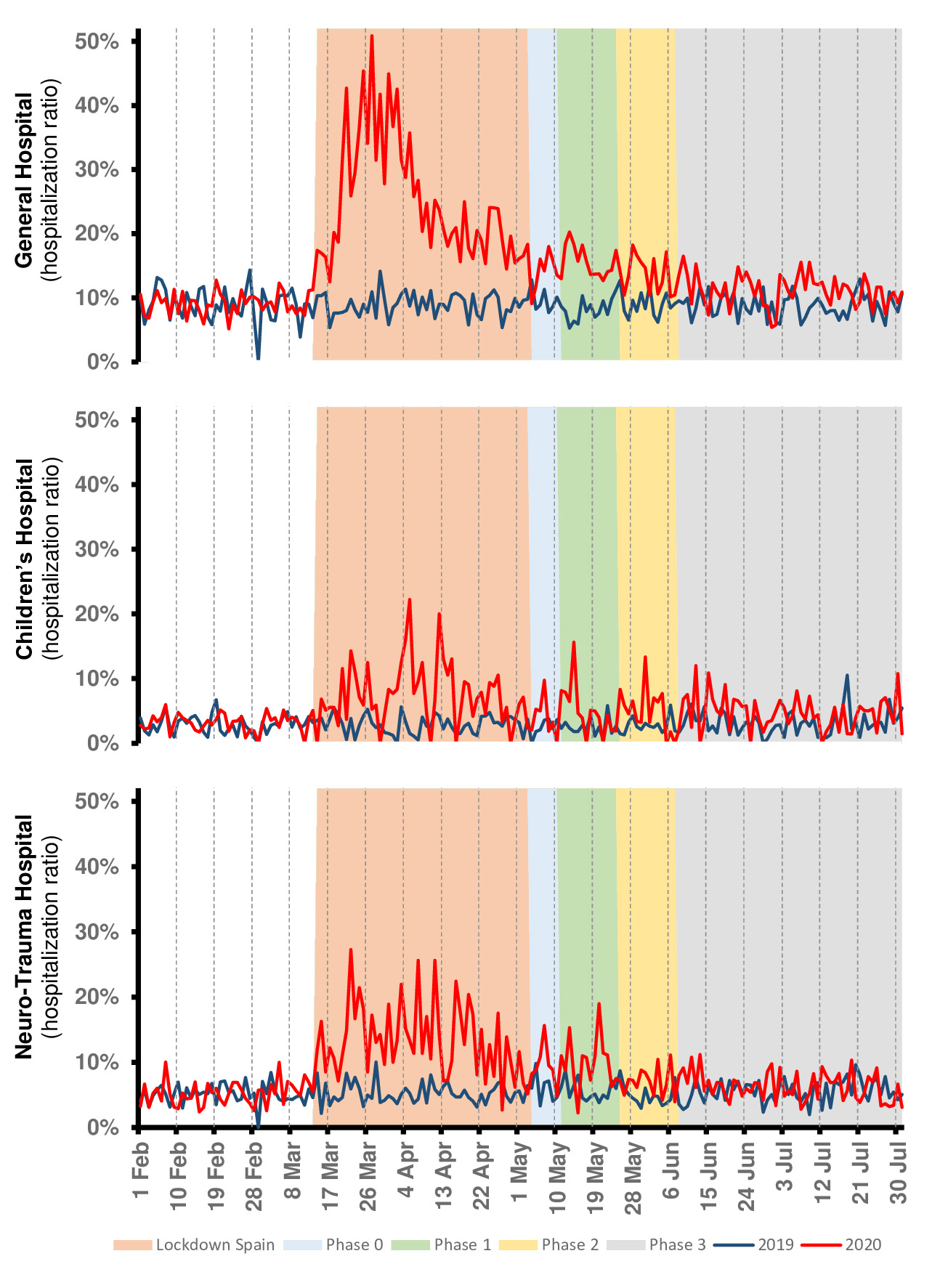
The hospitalization ratios were higher than the previous year with some differences among centers (Fig 2). These rose considerably during the lockdown and continued to show peaks until phase 3. Globally, all complex was affected by the changes in the new patters of use of the EDs, however, the complex which presented higher hospitalization ratio was GH. This ratio in GH’s ED reached almost 51% in March 27th 2020, being this ratio of 11% at the same day of 2019. Finally, they normalized concerning 2019 in that last phase.
Figure 2. Hospitalization ratios in the Emergency Departments of General Hospital, the Children’s Hospital and Neuro-Trauma Hospital of Virgen de las Nieves Hospital Complex.
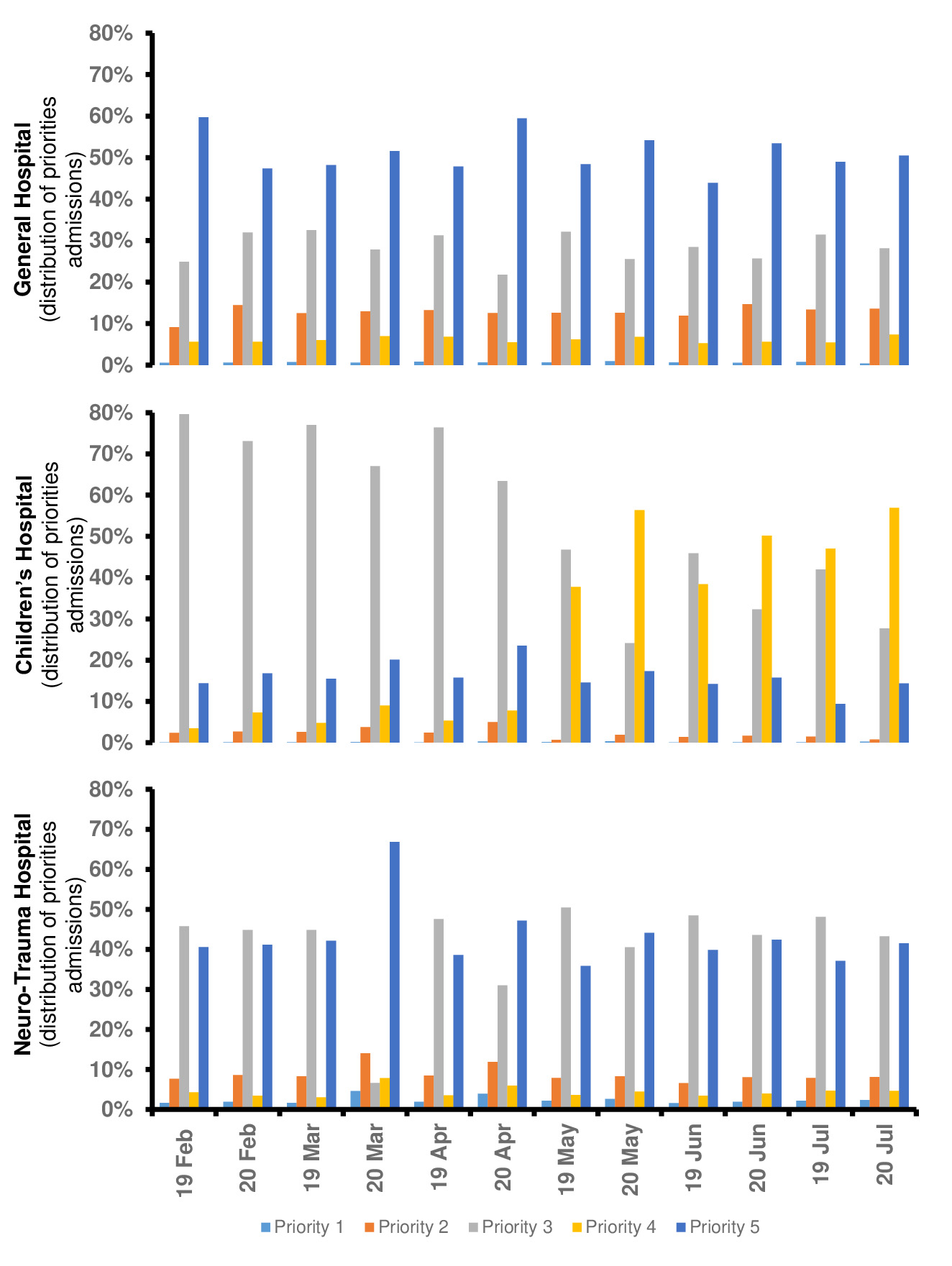
Fig 3 showed the distribution of the priorities in the EDs of the Virgen de las Nieves complex in the analyzed period, which showed some changes in its trend. While the highest priorities are always the same in GH (both years, priority 5), in CH and NTH it can be seen how in 2020 this highest priority changed depend on month and year (Fig 3).
Figure 3. Distribution of priorities admissions in the Emergency Departments of General Hospital, the Children’s Hospital and Neuro-Trauma Hospital of Virgen de las Nieves Hospital Complex
4. DISCUSSION
The COVID-19 has probably been the major challenge for National Health System in their recent history (9,10). A detailed analysis in pattern of use of EDs could allow us to partially understand their impact on society. Since these changes are likely to be here to stay, it would be interesting to assess them in depth to obtain useful information on population behavior in the pandemic’s context. Lockdown in Spain was declared on March 14th, after that, the de-escalation process happened in four phases in Granada: phase 0 (from May 4th), phase 1 (from May 11th), phase 2 (from May 25th), and phase 3 (from June 8th).
The SNHS ensures the health care of all the Spanish citizens; it is based on the Beveridge Health Care System (BHCS), where the health system is financed by taxes and does not involve co-payments for using the EDs. This universal health care system has evident benefits for the population but can imply a misuse of the system, particularly in the emergency room, where no appointment is needed to get medical attention (11,12,13). The current study sought to identify the possible influences of COVID pandemic on the pattern of use of the EDs, with special emphasis on the BHCS, trying to provide scientific evidence to help us better understand its effects on the health care system and allow us to develop better health care plans.
Different authors (13,14) from countries with BHCS, such as Italy, reported a general reduction of referrals to the EDs during the first wave of the COVID pandemic; varying the decrease with respect to previous years from 34.4% to 46.3%. Our figures were consistent with them showed an overall reduction in EDs admission of 38.83% in 2020 compared to 2019.
The influence of COVID on pediatrics attendance pattern to EDs showed engaging data as well. Different studies revealed a decreased in children attending from 27.11% to 88 % in 2020 compared to previous years reduction of 54.59%. Interestingly in our CH’s ED, there was a decreased in attendance to the EDs a week before the Spanish lockdown, possibly this can be explained because parents were the most sensible and foresighted due to the international context.
Bellan et al.(13) and Ojetti et al.(14) revealed a rise in hospitalizations ratio from 2019 (16.9%) to 2020 (35.5%)(13) or from 2018 and 2019 (27.7% and 26.4%, respectively) to 2020 (42.9%)(14). Our hospitalizations ratio in patients attending the ED of the GH was overall higher than in the same period of the previous year and reached almost 51% around March 25-27th 2020, in the NTH the higher ratio (27.3%) was reached on similar dates (March 22th 2020). Therefore, these figures might suggest a greater severity of patients attended in the ED during the first wave of the COVID-19 pandemic (14).
Concerning priorities, if we compare month on month in each year, changes in trend CH and NTH’s EDs were identified; while no notable changes were observed in GH’s ED. In the GH’s ED the priority 5 is the highest in all months (both years) but in the CH’s ED from May the highest priority changed. In the CH before May the highest priority was priority 3 (both years) but after May the most frequent priority was priority 3 in 2019 and 4 in 2020. In NTH’s ED the highest priority was priority 3 before March (both years), however, in the following months, the highest priority in 2019 is priority 3 but in 2020 is priority 5. This change in pattern of use continued until June.
If we analyse our data in more depth, we can obtain more useful information. During March 2020, priorities 4 and 5 increased and priorities 1 and 2 remained stable in CH’s ED, while priority 3 decreased. This could be explained in part because urgent (priority 3) pediatric cases did not attend as usual because of the fear of contagion. Nevertheless, in April and May 2020 priority 2 increased significantly compared with the same months of 2019 (2.5% April 2019 vs 5% April 2020; 0.7% May 2019 vs 1.9% May 2020). A plausible explication for these changes might be that some of the urgent cases who did not attend in Mach, with non-resolved and even worse clinical pictures, decided to attend in April and May. These changes appeared to achieve a “normal” situation in June with the end of the de-escalation process (1.4% June 2019 vs 1.7% June 2020).
In NTH’s ED, priority 2 and 5 increased in March 2020 at the expense of the decrease in urgent and standard cases (priority 3 and 4 respectively). Priorities 3 and 4 were usually patients with pathologies associated with minor (e.g. whiplash, muscular contracture, etc) and medium traffic accidents (not polytrauma); thus, they were reduced possibly by traffic closure. On the other hand, emergency care for serious cases was delayed, as can be seen in figures 2 and 3, possibly due to fear of COVID as previously mentioned.
Other authors have reported less attendance of patients with emergency pathology such as stroke (13–15), heart attack and sepsis (13,14,16) in accordance with our results. In addition, the complicated situation of cohabitation and mental exhaustion in Lockdown caused a growth in psychiatric pathologies (self-harm) (17). McIntyre et al. (17) found that the rate of presentation with self-harm dropped by 35% in the first two months of the COVID-19 pandemic and rose by 104% in the following two months. If a period of economic instability follows as predicted, it is likely that this will further impact the mental health of the population, along with rates of self-harm and suicidal behaviours. Thus, it could be useful to investigate not only the long-term effect of COVID-19 but also the consequences of lockdown restrictions.
If we re-analyze our result globally, there are a few facts that stand out. The overall reduction of admissions and hospitalization were 38.83% and 10.55%, respectively. Both drops should be alike, however, they were not; the reduction in the number of hospitalizations did not correlate directly with the decrease in admissions. Probably, changes in the pattern of use of EDs is the main cause for these differences. Moreover, these data lead us to discuss about the BHCS. This health care system has been criticized because, in normal conditions, people attend ED not only when they suffer from a severe health problem, but also as a way to get quick and free access to medical care, which constitutes a misuse of the system. Our data suggest that the theory about the misused of EDs could be true. Nonetheless, we have not been able to confirm this hypothesis with our data. To confirm this hypothesis, future prospective and randomized studies should be performed.
These results made us consider several ideas. 1) The coming of COVID-19 seems a good opportunity to understand the flow of patients to the EDs in Spain, which is probably comparable to other countries with similar health systems. It is tempting trying to get quick and easy conclusions looking at these numbers, but understanding all the reasons behind this drastic reduction in the number of patients admitted to the EDs is much more challenging. Thus, we could expect some changes in the flow of patients to the ED due to this new situation. 2) The fear of contagion might be responsible for a decrease in the number of less severe cases (priority 4 and 5) and children; this may be the main factor to consider. 3) The lockdown itself could cause fewer cases due to road-traffic, work, and sports accidents. Nevertheless, severe emergencies due to strokes, heart attacks, acute abdomen, etc., should have maintained their numbers in general, even some increment in the cases related to cardiovascular events might be expected due to the sedentariness imposed to the population during the lockdown. Furthermore, COVID-19 cases would cause an increase in the numbers affecting both the ED’s admissions and the hospitalizations. These theories are supported by other authors (13,14,18,19) .
The COVID-19 pandemic has been an inspiration for many authors to analyze the flux of patients in the EDs (11,13,14,17–20). However, it is very difficult to analyze and compared their results due to their differences (short follow-up periods, different period of time, countries health care system or different type of hospital). In order to address these limitations, the current study shows a longer follow-up period, EDs of complete hospital complex (GH, CH and NTH) and a higher number of patients than other research works based on the same health system (BHCS) (13,14).
The main limitations of our study were its retrospective nature and its analysis limited to BHCS. Thus, we cannot make conclusions about effect of COVID on global health care system. Nonetheless, this focus on BHCS is a strength at the same time since allow us understand better what happened in others countries with the same health care system.
5. CONCLUSION
The COVID-19 constitutes one of the greatest challenges in modern medicine, with still unknown consequences, including its impact on the patterns and flow of patients in primary and hospital care. Understanding better these changes and the impact that COVID-19 has caused, will probably lead us to manage and use better our public health systems in the future.
ACKNOWLEDGEMENTS
The authors would like to thank all the health care workers in the analyzed hospitals for their work and efforts.
BIBLIOGRAPHIC REFERENCES
- ↑COVID-19 Map – Johns Hopkins Coronavirus Resource Center [Internet]. [cited 2021 Apr 7]. Available from: https://coronavirus.jhu.edu/map.html
- ↑Moazzami B, Razavi-Khorasani N, Dooghaie Moghadam A, Farokhi E, Rezaei N. COVID-19 and telemedicine: Immediate action required for maintaining healthcare providers well-being. J Clin Virol. 2020 May 1;126. DOI: 1016/j.jcv.2020.104345
- ↑Ohannessian R, Duong TA, Odone A. Global Telemedicine Implementation and Integration Within Health Systems to Fight the COVID-19 Pandemic: A Call to Action. JMIR Public Heal Surveill. 2020 Apr 2;6(2):e18810. DOI: 2196/18810
- ↑Bokolo Anthony Jnr. Use of Telemedicine and Virtual Care for Remote Treatment in Response to COVID-19 Pandemic. J Med Syst. 2020 Jul 1;44(7). DOI: 1007/s10916-020-01596-5
- ↑Contreras CM, Metzger GA, Beane JD, Dedhia PH, Ejaz A, Pawlik TM. Telemedicine: Patient-Provider Clinical Engagement During the COVID-19 Pandemic and Beyond. Vol. 24, Journal of Gastrointestinal Surgery. Springer; 2020. p. 1692–7. DOI: 1007/s11605-020-04623-5
- ↑Leibner ES, Stokes S, Ahmad D, Legome E. Emergency department COVID management policies: one institution’s experience and lessons learned. Emerg Med Pract. 2020 May 4;22(5):1.
- ↑Storm-Versloot MN, Ubbink DT, Kappelhof J, Luitse JSK. Comparison of an Informally Structured Triage System, the Emergency Severity Index, and the Manchester Triage System to Distinguish Patient Priority in the Emergency Department. Acad Emerg Med. 2011 Aug 1;18(8):822–9. DOI: 1111/j.1553-2712.2011.01122.x
- ↑Azeredo TRM, Guedes HM, Rebelo de Almeida RA, Chianca TCM, Martins JCA. Efficacy of the manchester triage system: A systematic review. Vol. 23, International Emergency Nursing. Elsevier Ltd; 2015. p. 47–52. DOI: 1016/j.ienj.2014.06.001
- ↑Fagoonee I, Pellicano R. COVID-19 brings the world economy to its knees. Minerva Med. 2020 Aug 1;111(4):297–9. DOI: 23736/S0026-4806.20.06603-3
- ↑Kickbusch I, Leung GM, Bhutta ZA, Matsoso MP, Ihekweazu C, Abbasi K. Covid-19: How a virus is turning the world upside down. 369, The BMJ. BMJ Publishing Group; 2020. DOI: 10.1136/bmj.m1336
- ↑Clavenna A, Nardelli S, Sala D, Fontana M, Biondi A, Bonati M. Impact of COVID-19 on the Pattern of Access to a Pediatric Emergency Department in the Lombardy Region, Italy. Pediatr Emerg Care. 2020 Oct 1;36(10):e597–8. DOI: 1097/PEC.0000000000002232
- ↑Naouri D, Naouri D, Ranchon G, Vuagnat A, Schmidt J, Schmidt J, et al. Factors associated with inappropriate use of emergency departments: Findings from a cross-sectional national study in France. BMJ Qual Saf. 2020 Jun 1;29(6):449–64. DOI: 1136/bmjqs-2019-009396
- ↑Bellan M, Gavelli F, Hayden E, Patrucco F, Soddu D, Pedrinelli AR, et al. Pattern of emergency department referral during the Covid-19 outbreak in Italy. Panminerva Med. 2020; DOI: 23736/S0031-0808.20.04000-8
- ↑Ojetti V, Covino M, Brigida M, Petruzziello C, Saviano A, Migneco A, et al. Non-COVID Diseases during the Pandemic: Where Have All Other Emergencies Gone? Medicina (B Aires). 2020 Oct 1;56(10):512. DOI: 3390/medicina56100512
- ↑Montaner J, Barragán-Prieto A, Pérez-Sánchez S, Escudero-Martínez I, Moniche F, Sánchez-Miura JA, et al. Break in the Stroke Chain of Survival Due to COVID-19. 2020 May 29;STROKEAHA120030106. DOI: 10.1161/STROKEAHA.120.030106
- ↑Pinto S. Coronavirus disease 2019 (COVID-19): Myocardial infarction and other coronary artery disease issues – UpToDate [Internet]. [cited 2020 Nov 7]. Available from: https://www.uptodate.com/contents/coronavirus-disease-2019-covid-19-myocardial-infarction-and-other-coronary-artery-disease-issues
- ↑McIntyre A, Tong K, McMahon E, Doherty AM. COVID-19 and its Effect on Emergency Presentations to a Tertiary Hospital with Self-Harm in Ireland. Ir J Psychol Med. 2020 Sep 30;1–20. DOI: 1017/ipm.2020.116
- ↑Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Vol. 4, The Lancet Child and Adolescent Health. Elsevier B.V.; 2020. p. e10–1. DOI: 1016/S2352-4642(20)30108-5
- ↑Raman R, Madhusudan M. Impact of the COVID-19 Pandemic on Admissions to the Pediatric Emergency Department in a Tertiary Care Hospital. Indian J Pediatr. 2020 Nov 4;1. DOI: 1007/s12098-020-03562-y
- ↑Bjørnsen LP, Næss-Pleym LE, Dale J, Laugsand LE. Pasienttilstromming i et akuttmottak i pavente av covid-19-pandemien. Tidsskr den Nor Laegeforening. 2020;140(8):1–5. DOI: 4045/tidsskr.20.0277
ARTICLE INFORMATION
Conflict of interests: The authors of this article declare that they have no conflict of interest with respect to what is stated in this work.
Corresponding: Javier Lacorzana, MD. Virgen de las Nieves University Hospital. Av. de las Fuerzas Armadas, 2 · 18014 Granada. E-mail: javilacor@gmail.com