Original
3D morphometric analysis of colon applied to a laparoscopic surgical approach. Cadaver study
Análisis morfométrico 3D de colon aplicado a un abordaje quirúrgico laparoscópico. Estudio cadaver
Actual Med. 2021; 106(814): 260-270 DOI: 10.15568/am.2021.814.or03
Recibido: 08/11/2021
Revisado: 07/12/2021
Aceptado: 06/02/2022
ABSTRACT
Objective: The aim of this study is to define the changes that occurred in certain segments of the colons of cadavers after subjecting them to the conditions that are used in laparoscopic surgery of the colon.
Methodology: Three cadavers were submitted to abdominal computerized tomography, first with no external, and then after the application of 15 mm of Hg of pneumoperitoneum and 15 degrees Trendelenburg, right or left lateral decubitus. Three-dimensional reconstruction of the images was performed for a morphological descriptive study of the pubic points, superior mesenteric artery, inferior mesenteric artery, hepatic flexure and splenic flexure.
Results: A total of 390 measurements were performed, 159 showed changes. The inferior mesenteric artery point modifications were the most strongly related to the other points. The transverse colon – pubic symphysis – descending colon angle depended on the pubic symphysis – descending colon distance, and the transverse colon – inferior mesenteric artery – descending colon angle depended on the inferior mesenteric artery – transverse colon distance.
Conclusions: The positional changes of the points studied were related to their attachment to the peritoneum, to the proximity of the neighboring viscera and to their location in the abdomen.
Keywords: Colorectal surgery; Tomography; Laparoscopy; Minimally invasive surgical procedures; Surgical procedures
RESUMEN
Objetivo: El objetivo de este estudio es definir los cambios ocurridos en ciertos segmentos colónicos de cadáveres tras someterlos a una cirugía laparoscópica de colon.
Metodología: Tres cadáveres fueron sometidos a tomografía computarizada abdominal, primero sin externa presión, y luego con aplicación de 15 mm Hg de neumoperitoneo y 15 grados Trendelenburg, en decúbito lateral derecho o izquierdo. Se realizó reconstrucción tridimensional de las imágenes para un estudio morfológico descriptivo de los puntos púbicos, arteria mesentérica superior, arteria mesentérica inferior, ángulo hepático y ángulo esplénico.
Resultados: Se realizaron un total de 390 mediciones, 159 mostraron cambios. Las modificaciones de los puntos de la arteria mesentérica inferior fueron las más fuertemente relacionadas con los otros puntos. El ángulo del colon transverso – sínfisis púbica – colon descendente dependía de la sínfisis púbica – distancia del colon descendente, y el ángulo del colon transverso – arteria mesentérica inferior – colon descendente de la distancia entre la arteria mesentérica inferior y el colon transverso.
Conclusiones: Los cambios posicionales de los puntos estudiados se relacionaron con su inserción al peritoneo, con la proximidad de las vísceras vecinas y con su ubicación en el abdomen.
Palabras clave: Cirugía colorrectal; Tomografía; Laparoscopia; Procedimientos quirúrgicos mínima- mente invasivos; Procedimientos quirúrgicos.
Leer Artículo Completo
INTRODUCTION
Colon morphology has been extensively described in classical treatises of human anatomy (1,2) and has been related to both visceral and bony neighboring structures. (3,4) There is considerable anatomical variability of the colon, which can mostly be explained by embryological development. The rotation of the intestinal loops influences the location of the different segments. (5) The fusion of the peritoneal layers that occurs during the formation of the mesos and coalescence fascia can influence the length of certain sections of the colon and the positioning of its angles. (6)
The anatomical study of the colon has employed analytical methods based on radiological images and the resulting three-dimensional reconstructions, including computerized tomography (CT), nuclear magnetic resonance (MRI) or virtual colonoscopy (CT-colonoscopy). (7, 8, 9, 10) With these techniques, it is possible to analyze how age, sex, body mass index and pelvic diameter can influence the morphology, the disposition of fixed points or the intraluminal volume of the colon, among other parameters, (11) and the anatomy of this organ can be studied by moving the patient from a supine decubitus position to a prone or lateral decubitus position, an adjustment that is highly applicable in clinical practice. (12, 13, 14)
During laparoscopic surgery of the colon, different decubitus positions have been proposed to facilitate the correct mobilization of the intra-abdominal viscera and thus achieve good colon exposure. (15) For example, to expose the sigmoid colon, the surgical table is placed in the Trendelenburg position, and to examine the splenic flexure and the descending colon, a certain degree of right lateral decubitus positioning is used. (16–17) Therefore, for a successful surgery, it is considered necessary to vary the position of the patient so that the disposition of the colon is also modified.
No reference has been found in the literature that specifically describes the changes in colon placement that result from changes in posture.
Advantages and limitations of the technique.
The main advantage of this technique is that it is possible an evaluation of morphological changes that appear in an organ, in different pathological conditions, or as the effect of an intervention strategy. Also, this technique provides an important means of quantifying aspects of shape variation and enable visualization of these shape differences in a framework that is independent of differences in size between objects or specific regions.
The main problem with small studies is interpretation of results, in particular confidence intervals and p-values. Another major limitation is that they can produce false-positive results, or they over-estimate the magnitude of an association. In this case, a larger confirmatory study is needed.
MATERIAL AND METHODS
In this study, we propose as a hypothesis that certain points of the colon change location depending on the decubitus position that is used and that these changes can be measured and analyzed using radiological methods with three-dimensional reconstruction.
Cadavers. Placement and manipulation
The study was performed at the Jesus Uson Minimally Invasive Surgery Centre with three cadavers, two females (cadavers 1 and 3) and one male (cadaver 2), embalmed using the Thiel technique. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/ or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The need for written and informed consent for use of the patients’ cadaver for research purposes was not required because of the retrospective study design and the requirement was waived by Clinical Research Ethics Committee of Aragón (CEICA). The use of the images and the retrospective collection of data were approved by the Clinical Research Ethics Committee of Aragón (CE PI17/O168); data confidentiality and permission of data review were provided in the hospital admission consent.
A Brilliance CT multi-cutter scanner was used (Philips Medical Systems, Nederland B.V). The image processing and measurement software used were OsiriX, Adobe Photoshop Elements 11 Editor and ImageJ.
A working protocol was established and repeated for the three cadavers. The cadavers were placed in the scanner on wooden wedges at a 15º angle to achieve the different postural changes. The pneumoperitoneum was created with a periumbilical Veress needle. Four 12-mm disposable trocars were placed in the epigastric periumbilical and both iliac fossa locations for the introduction of a 0° Storz scope and disposable forceps in the series required for the manipulation of the colon.
The ten series of the study were modified with different degrees of pneumoperitoneum and postural decubitus. Series 01 (BASELINE) was a control performed in supine decubitus without pneumoperitoneum. The remaining series were performed with 15 mm Hg of pneumoperitoneum. Series 02 (PNEUMOPERITONEUM) was performed in supine position. Series 03 (RIGHT SIDE) was performed with 15º right lateral decubitus positioning. Series 04 (LEFT SIDE) was performed with 15º left lateral decubitus positioning. In the following series, a 15º Trendelenburg tilt was applied.
Series 05 (TRENDELENBURG) was performed with a 15º Trendelenburg tilt. Series 06 (TRENDELENBURG AND RIGHT SIDE) included both Trendelenburg tilt and 15º right lateral decubitus positioning. Series 07 (TRENDELENBURG AND LATERAL LEFT) included Trendelenburg tilt and 15º left lateral decubitus positioning. In the last three series, manipulation of the colon was introduced by elevating the greater omentum and exposing the transverse colon. Series 08 (OMENTUM) only included the elevation of the greater omentum with 15º Trendelenburg tilt. Series 09 (OMENTUM AND RIGHT SIDE) added 15º right lateral decubitus positioning. Series 10 (OMENTUM AND LEFT SIDE) added 15º left lateral decubitus positioning. The same order of manipulation was always followed for all three cadavers.
Obtaining and processing CT images
Following the described protocol, DICOM images were obtained using 3-mm CT scan sections. These images were processed with OsiriX software. The colon surface was manually individualized in all sections, and its image density was modified to obtain three-dimensional reconstructions. Chromatic changes in the three-dimensional images were made using Adobe Photoshop Elements 11.
After bringing the three-dimensional images to the frontal plane, the reference points were marked for the proposed measures. These points were the anterior superior iliac spines (SPINE); the midpoint of the pubic symphysis (PUBIS); the root of the superior mesenteric artery (SMA); the root of the inferior mesenteric artery (IMA); the highest point of the colon in the right hemiabdomen, in the transition zone between the ascending colon and the transverse colon (HF); and the highest point of the colon in the left hemiabdomen, in the transition zone between the transverse colon and the descending colon (SA).
Morphometric study
The cadavers were always studied in the frontal position. These measurements were performed using the computer program ImageJ and were calculated in pixels, which were later transformed to centimeters, and in sexagesimal degrees. The reference measurement was the SPINE-SPINE distance. To minimize the possible degree of distortion that could result from modifying the cadavers’ position relative to supine decubitus, this measure was used to apply a correction factor in each series. Thus, the differences observed in this measure after the cadavers were successively repositioned were less than 2%. A correlation analysis was performed to assess the dependence of some variables on others.
RESULTS
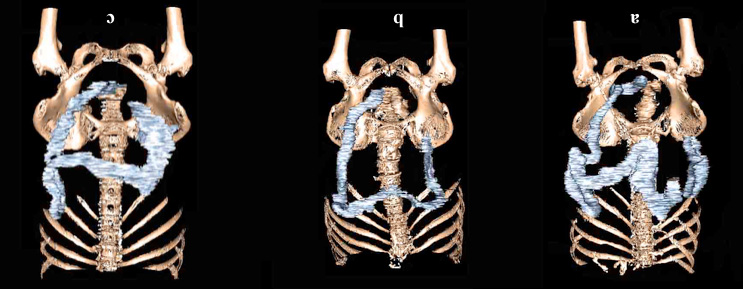
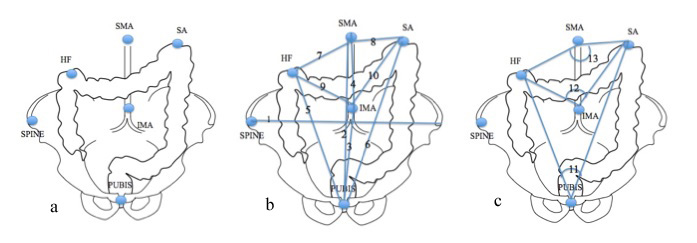
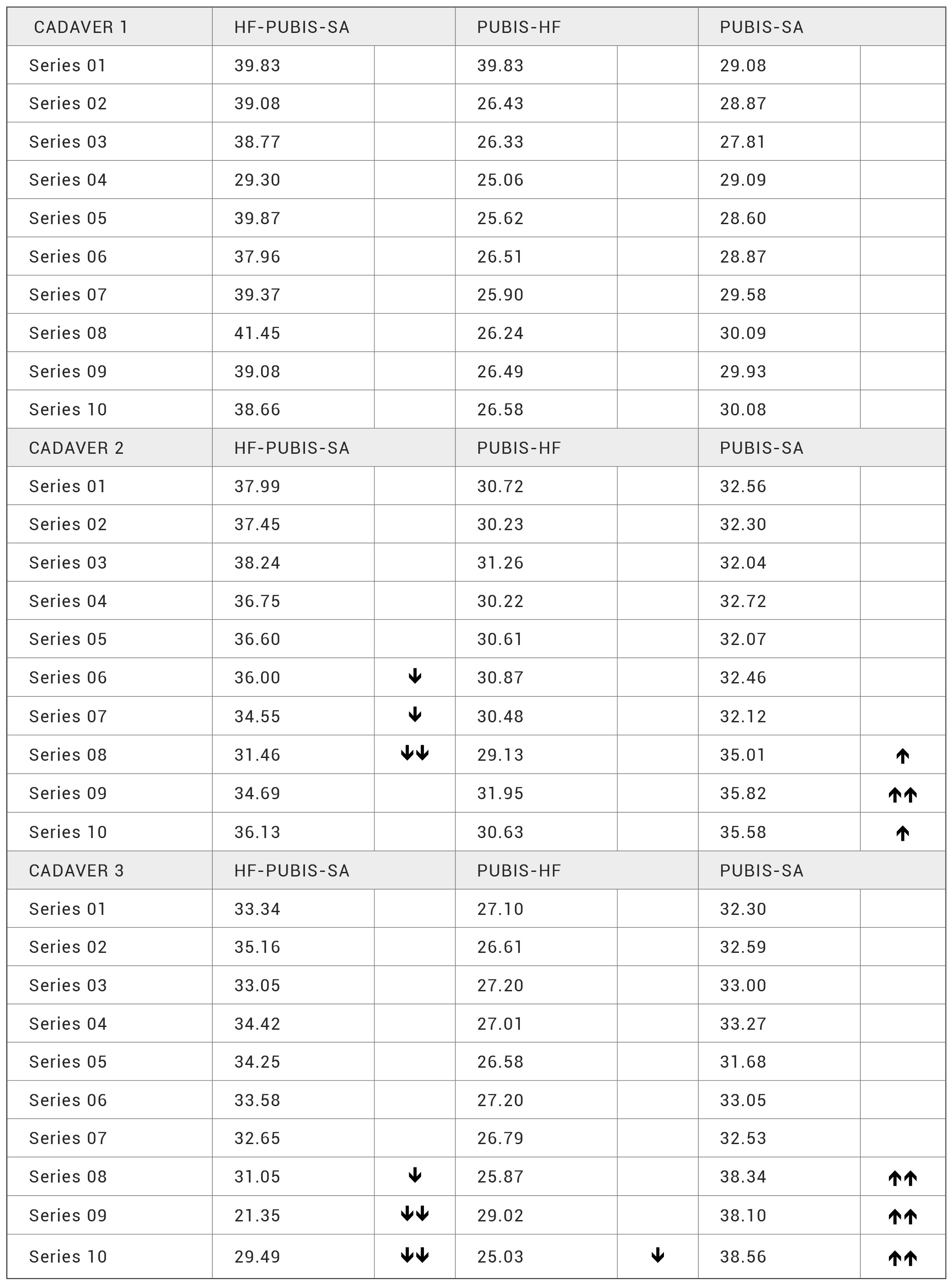
A total of 390 measurements were performed (Figure 1). Series 01 of the three cadavers was used as a reference and 159 measurements were modified more than 5% compared to this baseline. To systematize these results, we divided them into four sections depending on the angle and its components (Figure 2).
Figure 1. Three-dimensional reconstruction and chromatic change of the surface of the colon without pneumoperitoneum or any decubitus posture (Series 01). a: Cadaver 1. b: Cadaver 2. c: Cadaver 3.
Figure 2. Location of the variables proposed in the study as reference points and as measures of length and angle. a: Proposed reference points.
b: Measurements of the proposed lengths: SPINE-SPINE length, PUBIS-SMA length. PUBIS-IMA length. SMA-IMA length. PUBIS-HF length.
PUBIS-SA length. SMA-HF length. SMA-SA length. IMA-HF length. IMA-SA length. c: Proposed angle measurements: HF-PUBIS-SA angle. HFSMA-SA angle. HF-IMA-SA angle.
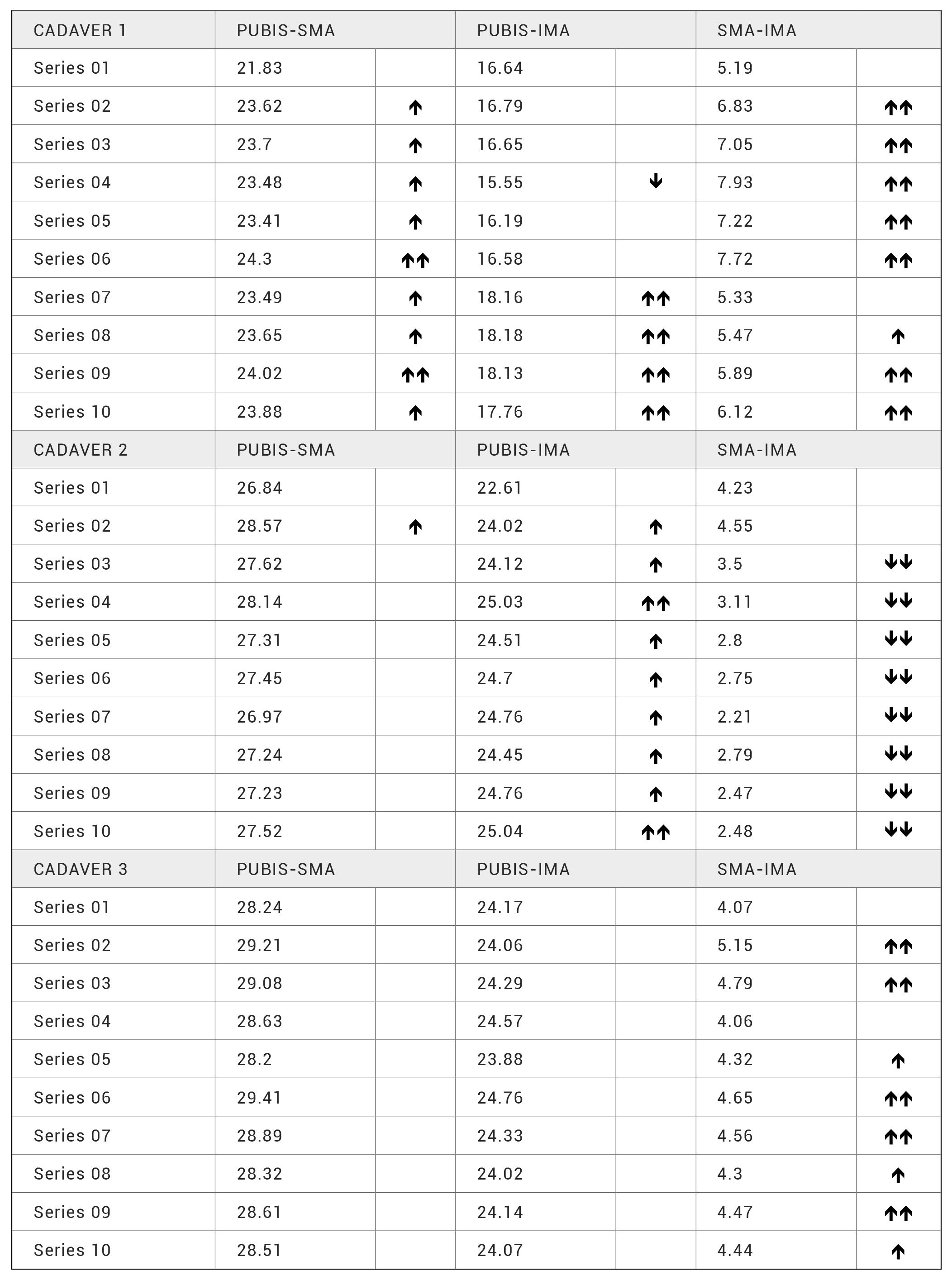
The PUBIS-SMA distance increased in all series in cadaver 1; in cadaver 2, it increased in series 02; in cadaver 3, it was not modified. The PUBIS-IMA distance increased in the last four series in cadaver 1 and decreased in series 04; in cadaver 2 it increased in all cases; in cadaver 3, it was not modified. The SMA- IMA distance increased in cadaver 1 in all series except for series 07; in cadaver 2, it decreased in all series except series 02, in which it did not change; in cadaver 3, it increased in all series except series 04, in which it did not change. The correlation test showed very high values between PUBIS-SMA and PUBIS-IMA (r = 0.94) and between PUBIS-IMA and SMA-IMA, although the correlation was negative (r = -0.86). The correlation between PUBIS-SMA and SMA-IMA was high and negative (r = -0.64) (Table 1).
Table 1. Variables related to the distances between PUBIS-SMA-IMA.
The HF-SMA-SA angle increased in all series in cadaver 1; in cadaver 2, it increased in series 02 and 04 and decreased in series 07, 08, 09 and 10; in cadaver 3, it only changes in series 09, in which it increased. The SMA-HF distance in cadaver 1 increased in series 02, 03, 05, 06, 07, 08 and 09 and decreased in series 04; in cadaver 2, it increased in series 04, 08 and 09; in cadaver 3, it increased in series 08 and 10 and decreased in series 09. The SMA-SA distance decreased in all series in cadaver 1; in cadaver 2, it decreased in series 02; in cadaver 3, it increased in series 03, 04, 08 and 10. The correlation test showed high values for the relationships among these variables (Table 2).
Table 2. Variables related to the HF-SMA-SA angle.
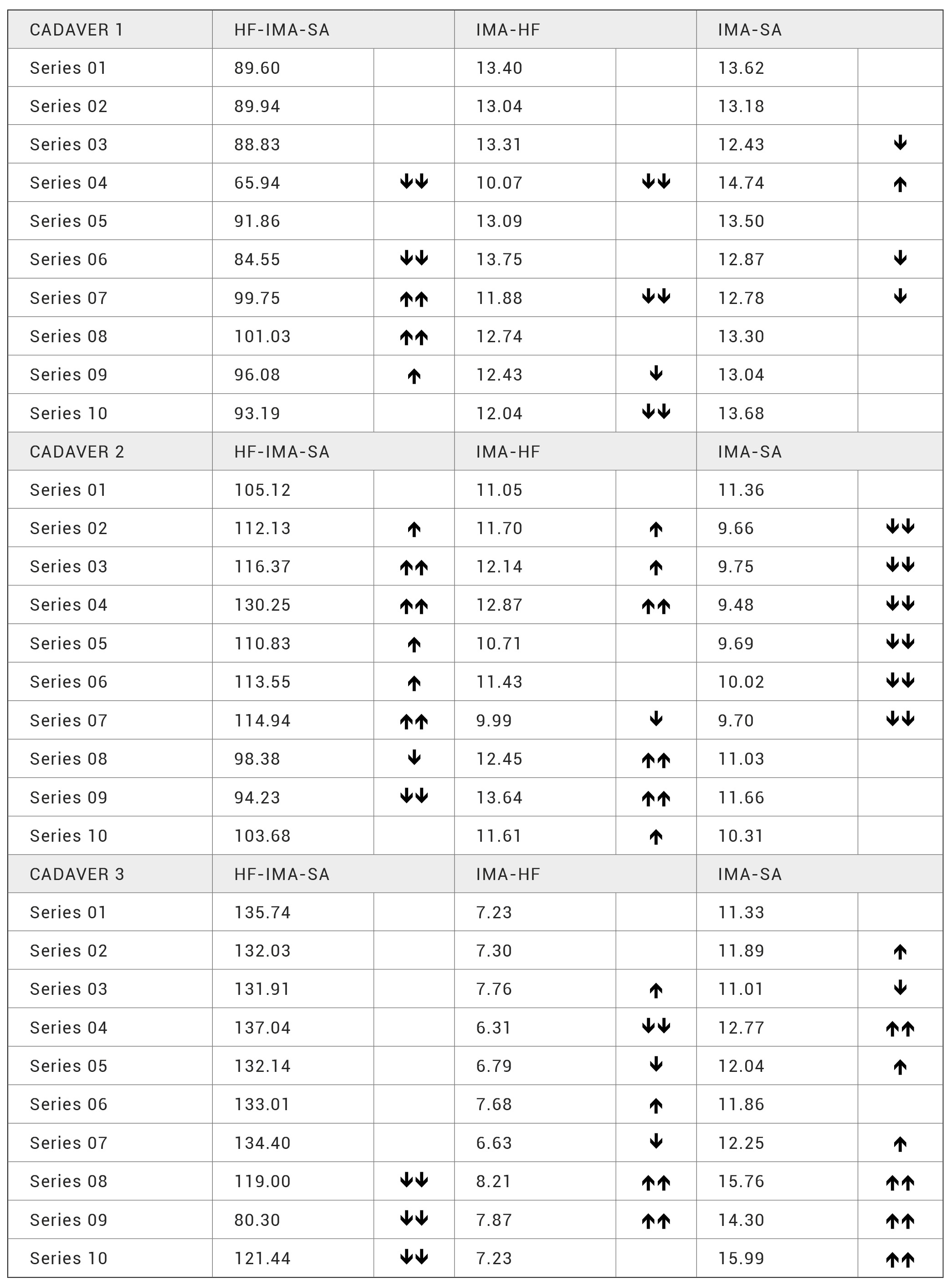
The HF-IMA-SA angle was modified in five series in cadaver 1 in various direction and magnitudes; in cadaver 2, it increased in all series from 02 to 07 and decreased in series 08 and 09. In cadaver 3, it only changed in the last three series, in which it decreased. The IMA-HF distance decreased in series 04, 07, 09 and 10 in cadaver 1; in cadaver 2, it increased in series 02, 03, 04, 08, 09 and 10 and decreased in series 07. In cadaver 3, it changed in seven series, with different directions and magnitudes. The IMA-SA distance in cadaver 1 changed irregularly in four series; in cadaver 2, it decreased in series 02, 03, 04, 05, 06 and 07; in cadaver 3, it did not change in series 06, decreased in series 03 and increased in the rest of the series. The correlation was strong and negative only for HF-IMA- AS and IMA-HF (r = -0.66) (Table 3).
Table 3. Variables related to the HF-IMA-SA angle.
The HF-PUBIS-SA angle did not change in cadaver 1; in cadaver 2, it decreased in series 06, 07 and 08; in cadaver 3, it increased in series 02 and decreased in the last three series. The PUBIS-HF distance did not change in cadavers 1 and 2; in cadaver 3, it increased in series 09 and decreased in series 10. The PUBIS-SA distance did not change in cadaver 1; in cadavers 2 and 3, it increased in series 08, 09 and 10. The correlation was only strong between HF-PUBIS-SA and PUBIS-SA, and the relationship was negative (r = -0.71) (Table 4).
Table 4. Variables related to the HF-PUBIS-SA angle.
Computer-aided anatomical analysis with the DICOM protocol is the most widely used medical imaging standard for the study and transfer of images. (18,19) This technology allowed us to examine the positions of different points of the abdominal viscera induced by different decubitus positions. (12-14) Our results are both descriptive and quantifiable. To perform interventions in laparoscopic surgery, the patient is positioned in decubitus to make the viscera targeted for the surgery more accessible. (15) However, the use of these decubitus positions is intuitive and is based on the positioning of organs. (13,15) Our results were not homogeneous, so the mobility of the different points studied could be related to more than one factor, such as fixations to the peritoneum and the proximity of other viscera.
DISCUSSION
Limitations of the study could include the small number of cadavers used and the method of fixation. Regarding the first, the performance of ten series in each of the three cadavers significantly increased the sample size of our study, so we consider the total number of measurements sufficient to initially assess the movements of the colon. Regarding the second point, the Thiel technique is the fixation technique used for training models for laparoscopic surgery. (20,21) Since it does not make the cadaver excessively stiff, it is considered ideal for the study of the mobility of the abdominal viscera. (20)
Our descriptive results are difficult to systematize when compared with the individual characteristics of the colon. Cadaver 1 had the longest colon and had the largest number of modified variables. Cadaver 2 had a very short colon and an intermediate number of modified variables. Finally, the colon of cadaver 3 had an intermediate length and the fewest modified variables. These results do not support the hypothesized relationship between size of the colon and the changes in the variables.
The correlations between the pubis and the mesenteric arteries and the mesenteric arteries with themselves suggest that when the distance from the pubis to the inferior mesenteric artery is modified, the distance and direction from the pubis to the superior mesenteric artery also changes. However, the distance from the pubis to the superior mesenteric artery and from the pubis to the inferior mesenteric artery is related to the distance between the two mesenteric arteries, although in a different direction. This leads us to propose that the distance between the two arteries tends to compensate for variations in the distance from the pubis to the superior mesenteric artery. Thus, the inferior mesenteric artery point could be more mobile than the superior mesenteric artery point. This proposal can be explained by the fact that the superior mesenteric artery is pinched by the pancreas at its outlet, increasing the mobility of the inferior pancreaticoduodenal artery as it enters the mesentery artery. These three characteristics make the superior mesenteric artery more limited in its movements than the inferior mesenteric artery, which simply attaches to the parietal peritoneum. (1-4)
According to the correlation test, the angle between the inferior mesenteric artery and the colic flexures increases as the distance from the mesenteric artery exceeds the hepatic flexure and vice versa. The hepatic flexure is in direct contact with the renal fascia since the peritoneal folds that attach it to the posterior wall are very short; this configuration confers limited mobility. In contrast, the splenic flexure is attached to the wall by the phrenicocolic ligament, which is a longer peritoneal fold and thus allows more mobility. (1-3) Therefore, when the inferior mesenteric artery is mobilized, the angle formed between it and the colic flexures is more closely related to the distance between the artery and the hepatic flexure, which has a fixed end, than to the distance from the splenic flexure, whose two extremes are laxer.
The variables related to the angle between the superior mesenteric artery and the colic flexures changed in different directions, and a high correlation index was not obtained. This may be because, as noted above, the superior mesenteric artery point depends on the pancreas, the pancreaticoduodenal artery outlet, and the mesenteric root, making it difficult to predict their movements in relation to the hepatic and splenic flexures. (3,4)
The variables related to the angle between the pubis and the colic flexures were the least modified, possibly because the pubis is a fixed point just as the hepatic flexure is and the size of this angle is inversely related to the displacements of its most mobile point, such as the splenic flexure. This may explain the high correlation index between the angle formed by the pubis and the colic flexures and the distance from the pubis to the splenic flexure.
Changes in the position of certain segments of the colon have been identified during virtual colonoscopy studies when the patient changes from supine to prone position. (12-14) These changes may be due to the need for insufflation of the colon to carry out the study. In fact, in endoscopic studies, the lateral decubitus position can be changed to the supine decubitus position to achieve a better intraluminal approach to the colic frame. (12)
Laparoscopy is currently the technique of choice for most surgical procedures on the colon. Many studies have been published comparing laparoscopic surgery with open surgery and showing the benefits of laparoscopic surgery. (22,23) The series established in the working protocol reproduced the different postural changes performed during surgery. The aim of lateral decubitus positioning is to displace the intestinal loops towards the corresponding side, obtaining a good exposure of the colon, and to attempt greater medial displacement of the hepatic flexure or the splenic flexure (according to the side) when performing correct traction. More mobile points, such as the ileocecal junction or even the descending colon-sigmoid junction, may have greater displacement.(16,17) Regarding our proposal, our quantitative results are imprecise. However, the correlation analysis allowed us to relate the displacements of the studied points to one another. In this way, we have associated these displacements with the mobility of the points according to their insertion in the peritoneum. A short insertion allows little mobility (hepatic flexure), in contrast with a long insertion (splenic flexure) or a less fixed insertion (inferior mesenteric artery). When the point studied was related to additional factors, such as the proximity of another organ or vessel (superior mesenteric artery), the displacement was more difficult to determine. Thus, when a distance is defined by a fixed point and a moving point, it is easier to determine its angle than if the segment is delimited by two moving points.
CONCLUSION
Colon undergoes changes in the location of certain segments in the application of factors such as position changes and pneumoperitoneum pressure. These changes, which can be measured by three- dimensional reconstruction images, could be related to their fixations to the peritoneum, to the proximity of the neighboring viscera and to their location in the abdomen. (24)
BIBLIOGRAPHIC REFERENCES
-
- ↑Barussaud ML, Danion J, Castagnet M, et From ana- tomy to laparoscopic surgery, or how to reconcile sur- geons to embryology. Surg Radiol Anat 2015; 37:393–8.
- ↑Gao A, Li H, Xiao-Bing Z, et Accuracy and efficiency of computer-aided anatomical analysis using 3D visualiza- tion software based on semi-automated and automated segmentations. Ann Anat 2017; 210:76–83.
- ↑Gallot Anatomie chirugicale du côlon. EMC techniques chirurgicales. Appareil digestif 2006; 40-535.
- ↑Bourgouin S, Bège T, Lalonde N, et Three-dimensional determination of variability in colon anatomy: applica- tions for numerical modeling of the intestine. J Surg Res 2012;178:172–80.
- ↑Hong D, Tavanapong W, Wong J, et 3D Reconstruc- tion of virtual colon structures from colonoscopy images. Comput Med Imaging Graph 2014;38:22–33.
- ↑Hunter A, Eisma R, Lamb Thiel embalming fluid a new way to revive formalin-fixed cadaveric specimens. Clin Anat 2014;27:853–5.
- ↑Kim YS, Park SH, Ahn SD, et Differences in abdomi- nal organ movement between supine and prone positions measured using four-dimensional computed tomogra- phy. Radiother Oncol 2007;85:424–8.
- ↑Jeong YJ, Cho BH, Kinugasa Y, et Fetal topohistolo- gy of the mesocolon transversum with special reference to fusion with other mesenteries and fasciae. Clin Anat 2009;22:716–29.
- ↑Khashab MA, Pickhardt PJ, Kim DH, et Colorectal ana- tomy in adults at computed tomography colonography: normal distribution and the effect of age, sex, and body mass index. Endoscopy 2009;41:674–8.
- ↑Kim JY, Park SH, Lee SS, et al. Ascending colon rotation following patient positional change during CT colonography: a potential pitfall in interpretation. Eur Radiol 2011;21:353–9.
- ↑Netter Atlas de anatomía humana. Elservier Science, Barcelona. 2013.
- ↑Röttgen R, Fischbach F, Plotkin M, et Colon dissection: a new three-dimensional reconstruction tool for compu- ted tomography colonography. Acta Radiol 2005;46:222– 6.
- ↑Punwani S, Halligan S, Tolan D, et Quantitative as- sessment of colonic movement between prone and supi- ne patient positions during CT colonography. Br J Radiol 2009;82:475–81.
- ↑Pirlet I, Mercier N, Fabre JM. Tratamiento quirúrgico del cáncer del colon izquierdo. EMC – Técnicas Quirúrgicas – Aparato Digestivo 2014;30:1–11.
- ↑Rouvière H, Delmas A, Delmas Anatomía humana: descriptiva, topográfica y funcional. Masson, Barcelona. 2005.
- ↑Sadler TW, Langman J. Embriologia médica: con orientación clínica. Medica Panamerica, Buenos Aires. 2007
- ↑Shimizu F, Uehara M, Oatari M, et al. Three-dimensional visualization of the human face using DICOM data and its application to facial contouring surgery using free an- terolateral thigh flap transfer. J Plast Reconstr Aesthet Surg 2016;69:e1–e4.
- ↑Testut L, Latarjet Tratado de anatomía humana. Salvat, Barcelona. 1971.
- ↑Targarona EM, Balague C, Pernas JC, et Can we predict immediate e outcome after laparoscopic rectal surgery? Multivariate analysis of clinical, anatomic, and pathologic features after 3-dimensional reconstruction of the pelvic anatomy. Ann Surg 2008;247:642–9.
- ↑Takeda K, Hara T, Zhou X, et Normal model construc- tion for statistical image analysis of torso FDG-PET ima- ges based on anatomical standardization by CT images from FDG-PET/CT devices. Int J Comput Assist Radiol Surg 2017;12:777–87.
- ↑Valverde A, Mosnier Tratamiento quirúrgico del cáncer del colon derecho. EMC – Técnicas Quirúrgicas – Aparato Digestivo 2013;29:1–16.
- ↑Weeks JC, Nelson H, Gelber S, et Short-term quali- ty-of-life outcomes following laparoscopic-assisted co- lectomy vs open colectomy for colon cancer: a randomi- zed trial. JAMA 2002;287:321–8.
- ↑Wong KK, Sun Z, Tu J, et Medical image diagnostics based on computer-aided flow analysis using mag- netic resonance images. Comput Med Imaging Graph 2012;36:527–41.
- ↑[rs.3.rs-26613/v2] Fernando J, Escolar JD, Sánchez Mar- gallo F, García VE, Luesma MJ, Cantarero I, Fatás JA, Maestre J, López C,Usón 3D morphometric analysis of the colon applied to a laparoscopic surgical approach. Cadaver study. Researchsquare [Preprint]. May 15, 2020 [cited 2021 May 01] Available from: https://doi.org/10.21203/rs.3.rs-26613/v2.
ACKNOWLEDGEMENT
The authors wish to sincerely thank those who donated their bodies to science so that anatomical research could be performed. Results from such research can potentially improve patient care and increase mankind’s overall knowledge. Therefore, these donors and their families deserve our highest gratitude.
The authors thank the staff of the Department of Radiodiagnosis at the Hospital Royo Villanova of Zaragoza for their collaboration in obtaining the study images, as well as the staff of the Department of Microbiology, Preventive Medicine and Public Health at the University of Zaragoza for their help in performing statistical analyses.
ARTICLE INFORMATION
Conflict of interests: The authors of this article declare that they have no conflict of interest with respect to what is stated in this work.
Corresponding Author: Fernando Trebollé. Servicio de Cirugía General y de Aparato Digestivo. Hospital Royo Villanova Avda. San Gregorio 30 · 50015, Zaragoza. E-mail: jftrebolle@gmail.com