153
Ismael Khouly, DDS, MS, PhD
Treatment Options for the Atrophic Posterior Maxilla
English language publications were excluded. The search was
limited to studies involving human subjects. Restrictions were not
placed regarding the type of study design.
RESULTS
A total of 15 articles from reviewed journal published in
English were collected from a search performed using Medline
and Pubmed at the Waldman Library at the NYUCD Kriser Dental
Center. The following guideline tables are the result of this
literature review (TABLES 1, 2).
DISCUSSION
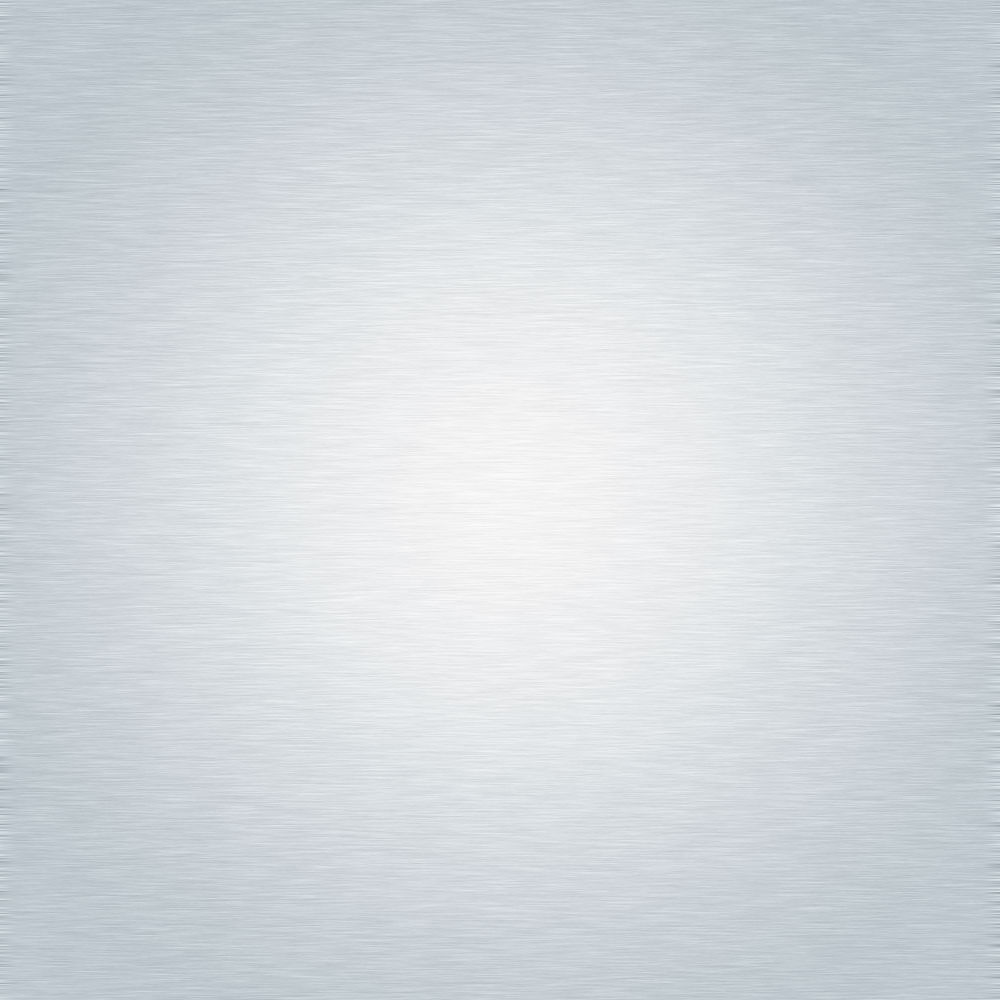
Due to the improvement of surgical techniques and the
progress of research in thefieldof biomaterials, excellent outcomes
have been reported for implant-supported rehabilitations in the
atrophic posterior maxilla in the past years. (21,22) The most
commonly utilized augmentation method for maxillary sinus
reconstruction was first presented by Tatum 19772, and published
by Boyne and James in 19801, using a window through the lateral
wall of the alveolus for sinus access. The LWSFE technique has
been widely described in the literature and is recommended with a
residual bone height less than 4 to 5 mm. This procedure has been
shown to be highly predictable for implant therapy with an overall
implant survival rate well beyond 90%. 5,6,7,23 Advantages of the
lateral window (LWSFE) approach to the sinus include direct view
of the sinus cavity, access to the Schneiderian membrane, and an
appropriate graft material placement15 (Fig.1, 2). However, this
procedure presents the disadvantages of prolonged time, cost,
and morbidity for the patient. (24,25)
To reduce complications and trauma that may occur
using the lateral wall approach, different techniques have been
proposed. The transcrestal approach to the maxillary sinus
(BAOSFE) has been advocated as ‘minimally invasive’ because of
the undisturbed vascularization of the graft and less postoperative
morbidity.4,9 According to standard protocol, the osteotome
technique should be used when the ridge height is greater than
4 to 5 mm where implants are placed simultaneously with the
elevation of the sinus floor (Fig.3). (3,4) Recently, a systematic
review of the literature showed that crestal sinus lift can be an
effective treatment option, reporting a mean weighted survival
rate of 95% after 5 years of function.26 The same review also
showed that the majority of failures occurred during the first
year after treatment. However, limitations of this procedure
include: limited accessibility and visibility for elevation of the
sinus membrane and inability to diagnose and treat membrane
perforations. (27,28,10) When the membrane is lifted more than
3 mm, the risk of membrane perforation increases significantly.
(29,30) The use of an endoscope has been proposed to diagnose
the membrane perforation during BAOSFE, increasing the cost
and time of the procedure. (29,30) Thus, in cases where crestal
height is 4-7 mm and an implant length of 10-13 mm is desired,
the sinus membrane will be lifted greater than 3mm, increasing
the risk of membrane perforation. An additional complication
reported following the use of osteotomes is paroxysmal positional
vertigo. (9)
Residual Bone
Height (mm)
Procedure
<4
Lateral wall, staged approach (delayed
placement)*
4-7
OASA Technique
8-10
Osteotome Technique
Table 1. Treatment options for atrophic posterior maxilla for single
implant. *Simultaneous implant placement if primary stability is
achieved (V-Shape sinus).
Residual Bone
Height (mm)
Procedure
<4
Lateral wall, staged approach (delayed
placement)*
4-7
Lateral wall, simultaneous placement
8-10
Osteotome Technique
Table 2. Treatment options for atrophic posterior maxilla for
multiple implants. *Simultaneous implant placement if primary
stability is achieved (V-Shape sinus).
Fig. 1a. Intraoperative view of lateral wall of the maxillary sinus
with Full thickness flap; Fig. 1b: Osteotomy of lateral wall window.
Fig. 1c: Placement of bone graftmaterial in the sinus cavity; Fig. 1d:
Resorbable membrane secured over the lateral window.
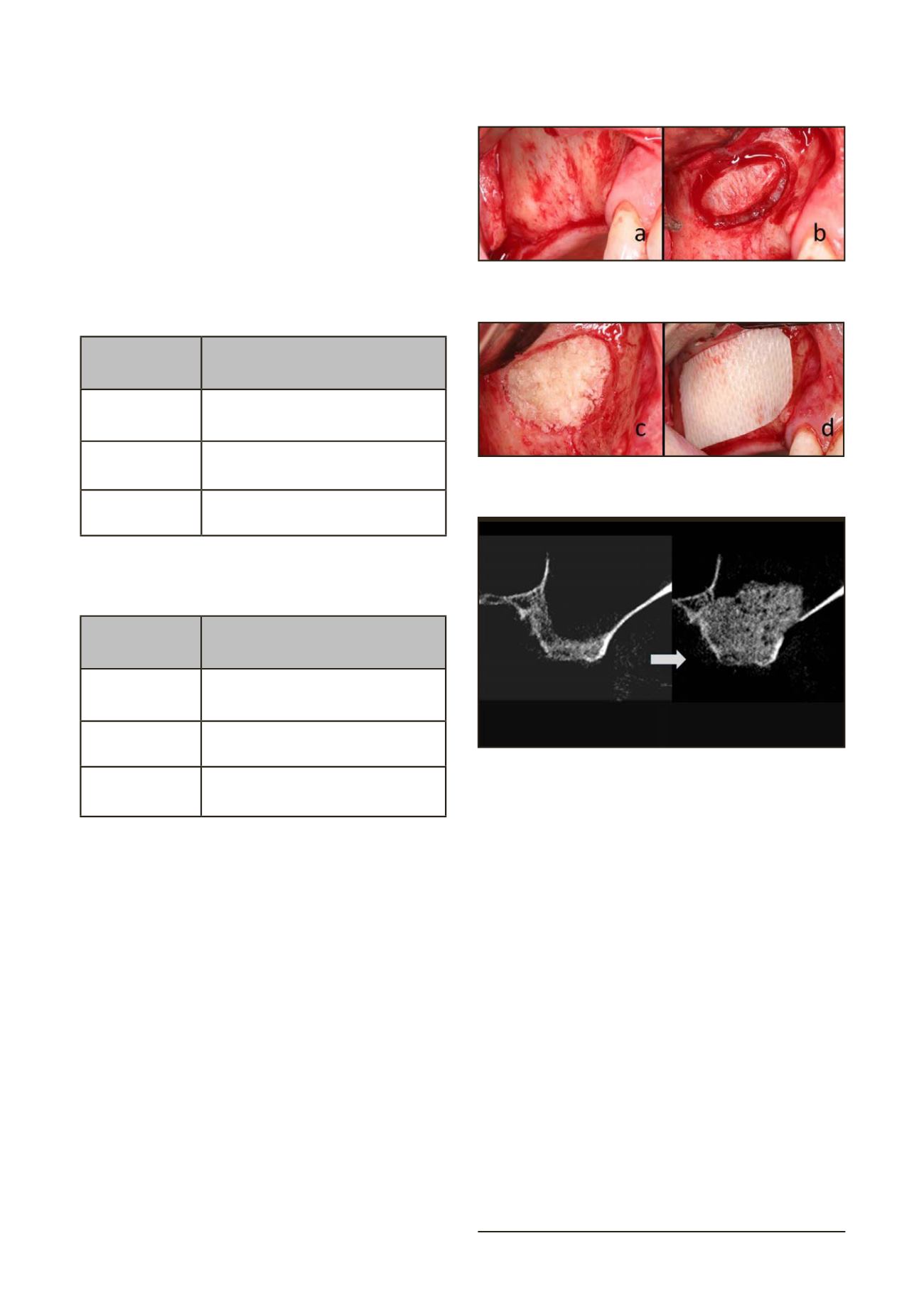
Fig. 2. Paraxial CT scans of sinus taken pre and post surgery.