44
original
SUPLEMENTO
Otoneurología 2014:
comprendiendomejor los trastornos vestibulares
Actual.Med.
2014; 99: (791). Supl. 44-60
and, for instance in toxic or traumatic cases, can be unnoticed
until thepatient recovers fromother injures.
Ward et al (1) based their criteria for diagnosis of BVH
on the fulfillment of all of the following elements: presence of
visual blurring with head movement; unsteadiness; difficulty
walking indarkness or unsteady surfaces and in a straight path;
and symptoms being at least “abigproblem” andpresent for at
least1year, in theabsenceofotherneurologicconditionsoreye
pathologic conditions affecting vision.
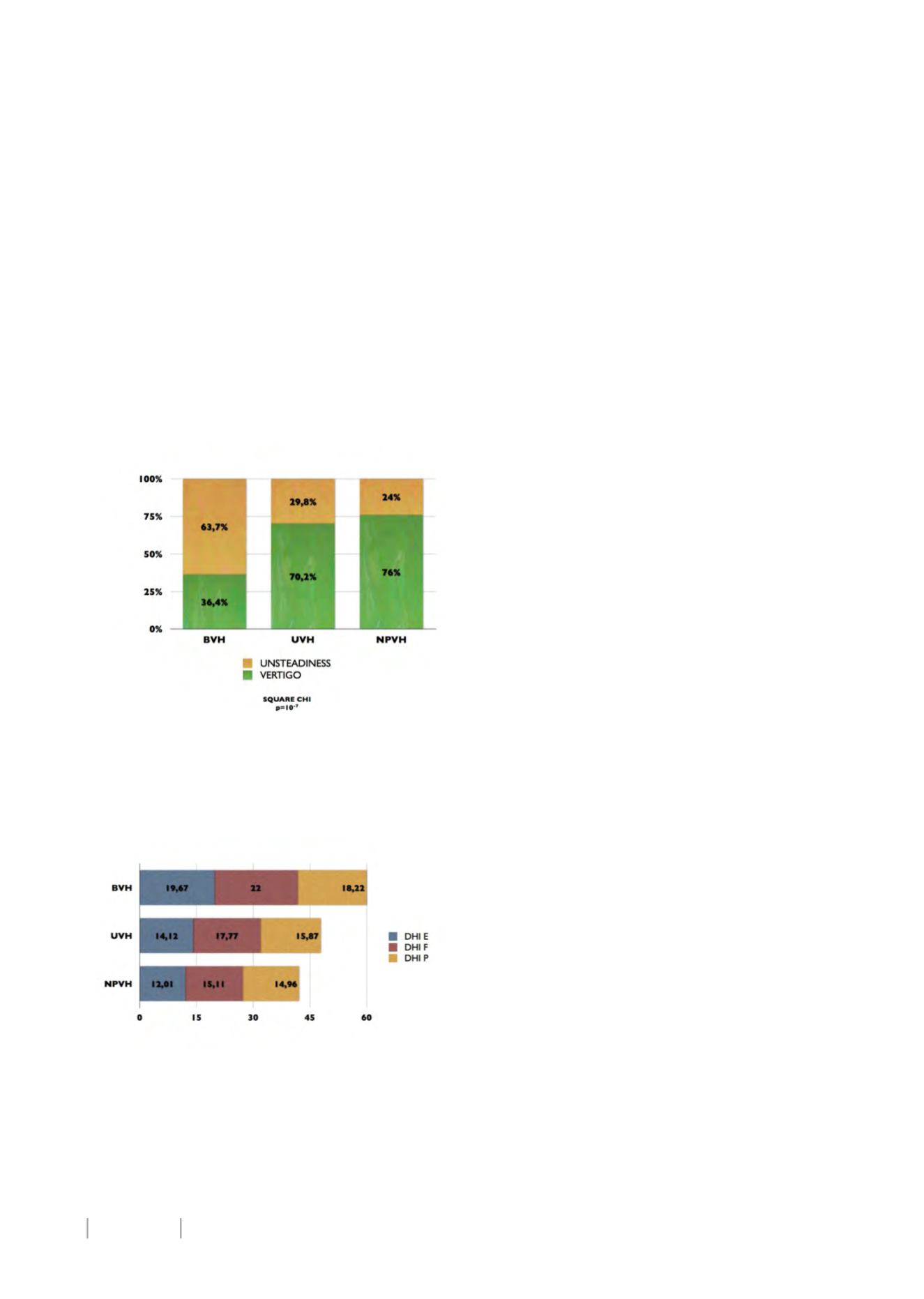
As seen in figure 2, most of the patients suffering from
BVH in our study population claimed to have unsteadiness as
main symptom, whereas the rest of the groups had anopposite
distribution. These differences were found to be statistically
significant (p=10
-7
for SQUARE CHI test). As for the temporal
course of symptoms, half of BVH patients (49,1%) described
a continuous sensation, albeit it worsened with movement.
UVH patients described a continuous sensation in amuch little
proportion (15,4%), and the same happened among NPVH
patients (11,1%). These differenceswere also found statistically
significant for the SQUARECHI test (p=10
-7
).
Figure2.Main symptomamonggroups
IMPACTONDAILY LIFE
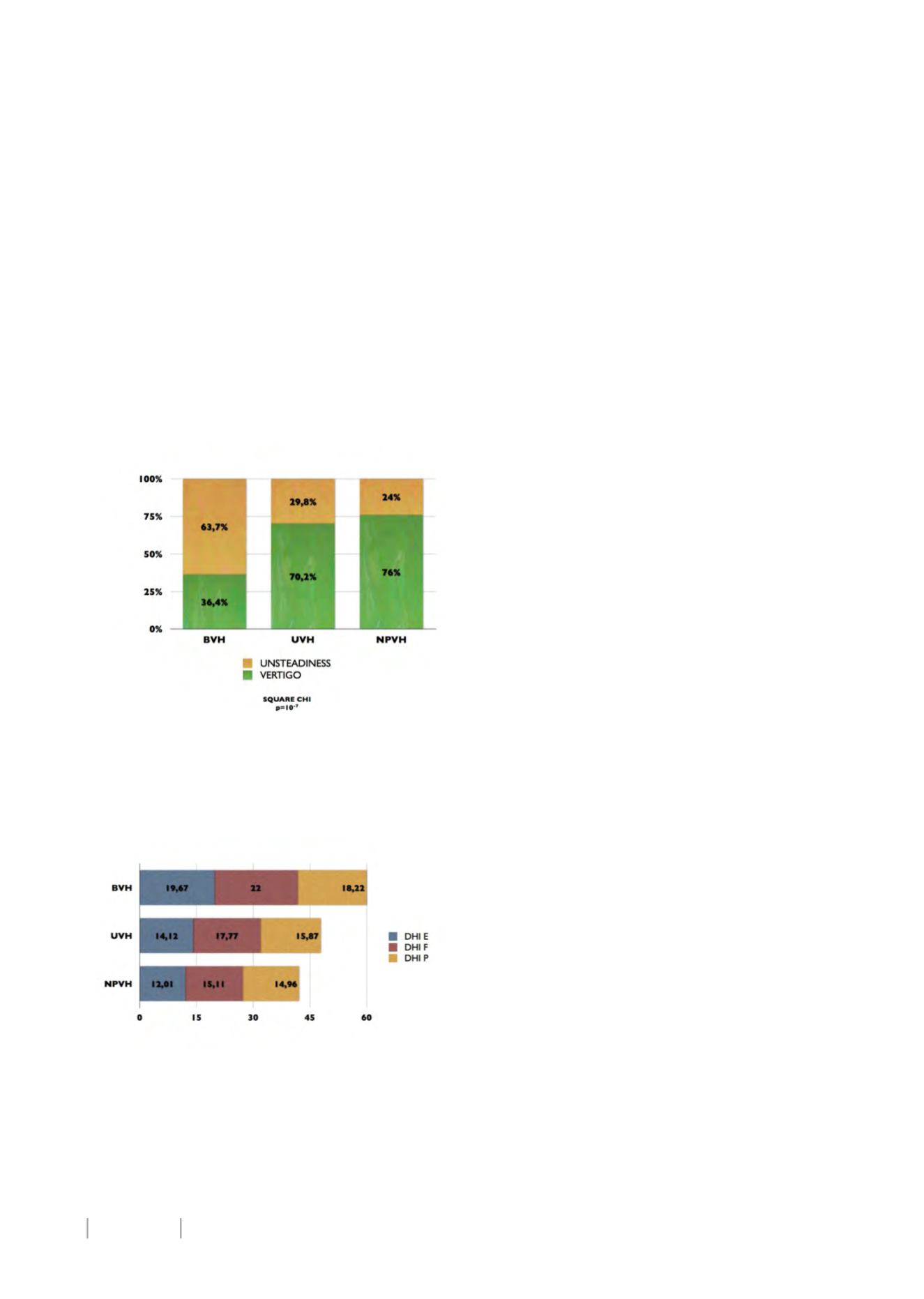
In figure 3 we represented mean scores for the Dizziness
Handicap Inventory (DHI) obtained ineachgroup.
Figure3.DizzinessHandicap Inventory scores
Emotional aspect of DHI was significantly worse (p=0,023
for Mann-Whitney test) among BVH patients than in UVH, and
also worse than among NPVH patients (p=0,001). In fact, all
the three components and the global score were significantly
different betweenBVH andNPVH groups (p=0,001 for functional
aspect and p=0,039 for physical aspect). As for UVH, differences
were statistically significant only for emotional component and
total score (p=0,043), addingnewevidence for assuming that the
findings described by Jáuregui-Renaud (13) and Gómez-Álvarez
(14) arenotonlypresent amongBVHpatients, but alsoappear to
be speciallymarked in this group.
Regarding daily impact, Ward et al (1) demonstrated an
increased risk of handicapped common activities, such as riding
on an escalator ormovingwalkway (odds ratio=8,1), going upor
down aflight of stairs (odds ratio=27,2-29,2), social activities like
visiting friends (odds ratio=11,5), or attending school or work
(odds ratio=19).
These authors also describe the finding of several other
difficulties related to improper use of visual or proprioceptive
confusing information, such as bumping when walking through
doorways or going through tunnels, and, specially, an increased
fall risk for these patients, as 87,8%had fallen in the last 5 years
because of their unsteadiness problem. In fact, age-adjusted fall
risk of their study population was 9 times greater than that of
otherdizzy respondentsand31timesgreater than their reported
national average.
DIAGNOSIS
Some considerations must be weighed when suspecting a
BVH, inorder to concludeonanaccuratediagnosis, evenwithout
any sort of assistant technology.
First, physiology and, most importantly, effect of the
vestibulo-ocularreflex (VOR)asgazestabilizermustbeaddressed.
When a normal VOR is present, head rotations are almost
instantly compensated by equal eye rotations in the opposite
direction. This system is extremelyefficient as its latency is about
10ms (14), and there is no possible substitution for this system,
if it is impaired, able to compensate headmovements in such a
short delay.
Thus, when VOR is not functioning correctly, eyes trend to
followhead at the beginning of its rotation, and afterwards, due
tovisual reflex, return tofixate the targetwitha rapidmovement
called saccade.
This saccade, that may be visible for the examiner, can be
used for diagnosis purposes, as it is a sensible sign of vestibular
loss (15).
As eyes drift from the target, it slips from the retinal
maximum visual acuity point for a moment, until drifting is
compensatedby the saccade, so, as adirect consequenceof VOR
impairment, there is a moment of blurry vision. This temporal
worseningofvisualacuitycanalsobeused fordiagnosispurposes,
asdescribedbyDemer andHonrubia (16).
Finally, it is not difficult to understand that, if no vestibular
information is available, balance without both visual and
proprioceptive inputs is not possible. This condition can be
achievedduring theperformanceof aRomberg test on foamand
witheyes closed (17).
PHYSICALEXAMINATION
These three considerationsweregathered ina recentpaper
authored by Petersen et al (18), who describes clinical diagnosis
of BVHasbasedon threebedside tests:
1.- Head impulse test (HIT):
firmly holding the head, the
examiner ask the patient to focus on a target and then, forces
fastpassive rotationsof theheadwithanapproximateamplitude
of 10-20º and, at least 120º/s. If VOR is working normally, eyes
move immediately on the opposite direction keeping focus on
the target, whereas, when VOR is impaired, head movement
towards theaffectedsidecannotbecompensated for suchabrisk
rotation, soeyes driftoff the target andmust performa catch-up
saccade. In thecaseofBVH, saccadescanbedetectedwhenhead
is rotated toboth sides.
Thereare two typesof saccades,dependingon their latency.
Saccades that occur within the rotation are called “covert”, and