45
Otoneurología 2014:
comprendiendomejor los trastornos vestibulares
SUPLEMENTO
original
Actual.Med.
2014; 99: (791). Supl. 45-60
those happening after the head movement are called “overt”.
Overt saccades are usually visible for the examiner without any
assistant technology, but, as we will address later on, covert
saccades arenot perceptible to thenakedeye.
2.- Dynamic visual acuity (DVA):
first, patient’s visual
acuity is measured using a standardized chart, such as Snellen
chart (19) or similar, manufactured following the guidelines
established by the International Council of Ophthalmology in
1984 (20). Afterwards, the same test is performedwhilemoving
the patient’s head alternately to both sides at 0,5-2Hz. Normal
subjects typically are able to maintain same or similar visual
acuity (losing nomore than 1 or 2 lines) (21), but when VOR is
absent, suchas inaBVH, visual acuity isdrasticallydiminished.
3.- Romberg test on rubber foam:
Romberg’s test is a
commonlyperformed testduring theneurological examination to
evaluate the integrityofdorsal columnsof the spinal cord.Moritz
Heinrich vonRomberg first described it in the early 19th century
(22). Positive result is considered when the patient is unable to
stand still with feet together andeyes closed. However, although
it isacommon test for theevaluationofdizzypatients, ithas little
specificityor sensitivity for vestibular loss.
Inorder to improve specificityand sensitivity, andespecially
in the caseof BVH, the test isperformedhaving thepatient stand
on foam. Adding this circumstance, vestibular input is the only
reference for balance, and, when there is impaired function in
both sides, patient isunable to remain still.
Sensibilityof HIT for diagnosingBVHhas beenestimated as
84%, while specificity was found to be 82% in a study authored
by Schubert et al (23). Nevertheless, this exploration might be
significantly conditionedbyexpertiseof theexaminer (19).
Vital et al (24) affirmed that DVA test sensitivitywas 100%,
specificitywas94%, andaccuracywas95%,with search-coil head
impulse testingusedas a reference.
Foamposturographysensitivitywas79%andspecificity80%
for detectingBVH (18).
COMPLEMENTARYTESTS
Although BVH can be relatively easy to diagnose just with
a thorough physical examination, there are some tests that can
be performed, either to confirm the suspicion or establish a
differential diagnosis, or to look for theexact etiology.
1.- Rotary Chair Tests.-
classically considered the gold
standard for diagnosing bilateral vestibular loss. During this test,
the patient sits, with head fixed and tilted 30º down, on a chair
that delivers two types of stimuli (25): Sinusoidal (which involves
rotating the chair so that itmoves sinusoidally toboth sides) and
impulse (which involves suddenly changing chair velocity). This
test examines both labyrinths at the sametime, and is useful not
only for diagnosis, but also to followup the compensation.
2.- Caloric Test.-
usuallymore available for clinical use, due
toeconomicaland logistic issues,calorictest is,probably, themost
commonlyusedexamination forBVHdiagnosis. It stimulateseach
labyrinth separately, giving a good evaluation of the vestibular
function for low frequency angular movements. Irrigating with
ice water can somehow increase its sensitivity, but, usually, the
test is performed instilling water 7 degrees above or below the
body temperature and comparing the response between ears,
andbetweennystagmusdirections. This test isuseful todiagnose
BVH, but unable to measure its extent (as it only assesses low
frequency rotation) or toevaluate compensation (26).
3.- Vestibular EvokedMyogenic Potential (VEMP) Testing.-
determines if the saccule, and the inferior vestibular nerve and
central connections, areworking normally. This potential derives
from the remnant sound sensitivity observed in the saccule, and
is known todisappearwhen this structureor its neural pathways
are impaired. It isnot supposed tobeofuse for recoveryor follow
up (26).
4.- Video Head Impulse Test (VHIT).-
as described by
MacDougall et al (26) andmodified for clinical practice, patient is
instructedtofixateadotonascreenat91cmdistance indim light.
20 horizontal head impulses to each side are manually applied
with unpredictable timing and direction. Peak head velocity of
the impulses should be at last 120º/second, since below that
frequencysmoothpursuitpathways(ratherthanVOR)areelicited.
This test can diagnose BVH bringing unique information about
the functioning of VOR at high frequency rotations, and, more
importantly, gives new and promising expectatives on recovery
and compensation processes measurement. Batuecas-Caletrio
et al (27)
showed a clear correlation between saccades pattern
and quality of life and subjective symptoms, finding that when
this pattern changed along follow up, symptoms and handicap
also evolved. As for assessing recovery and compensation with
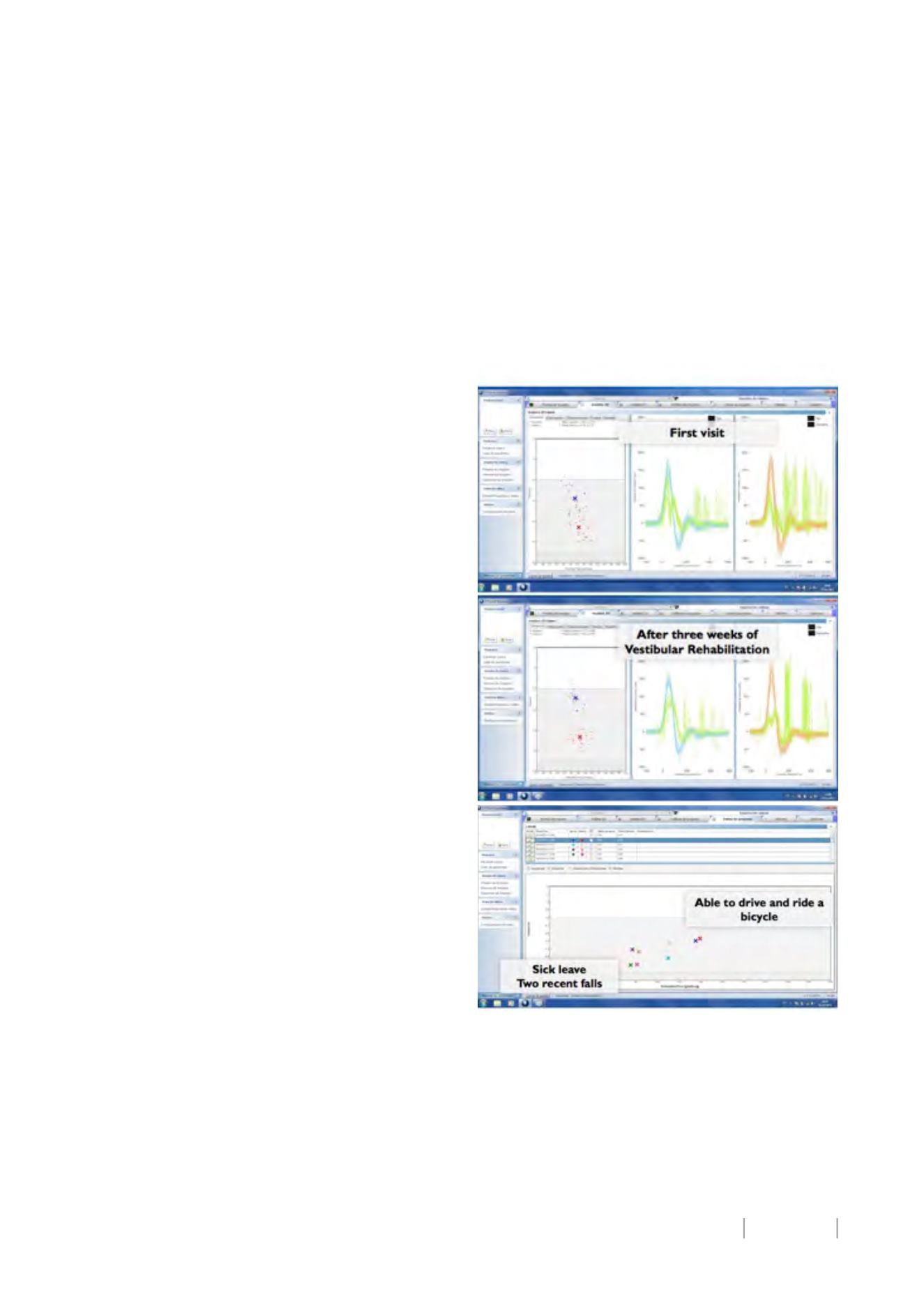
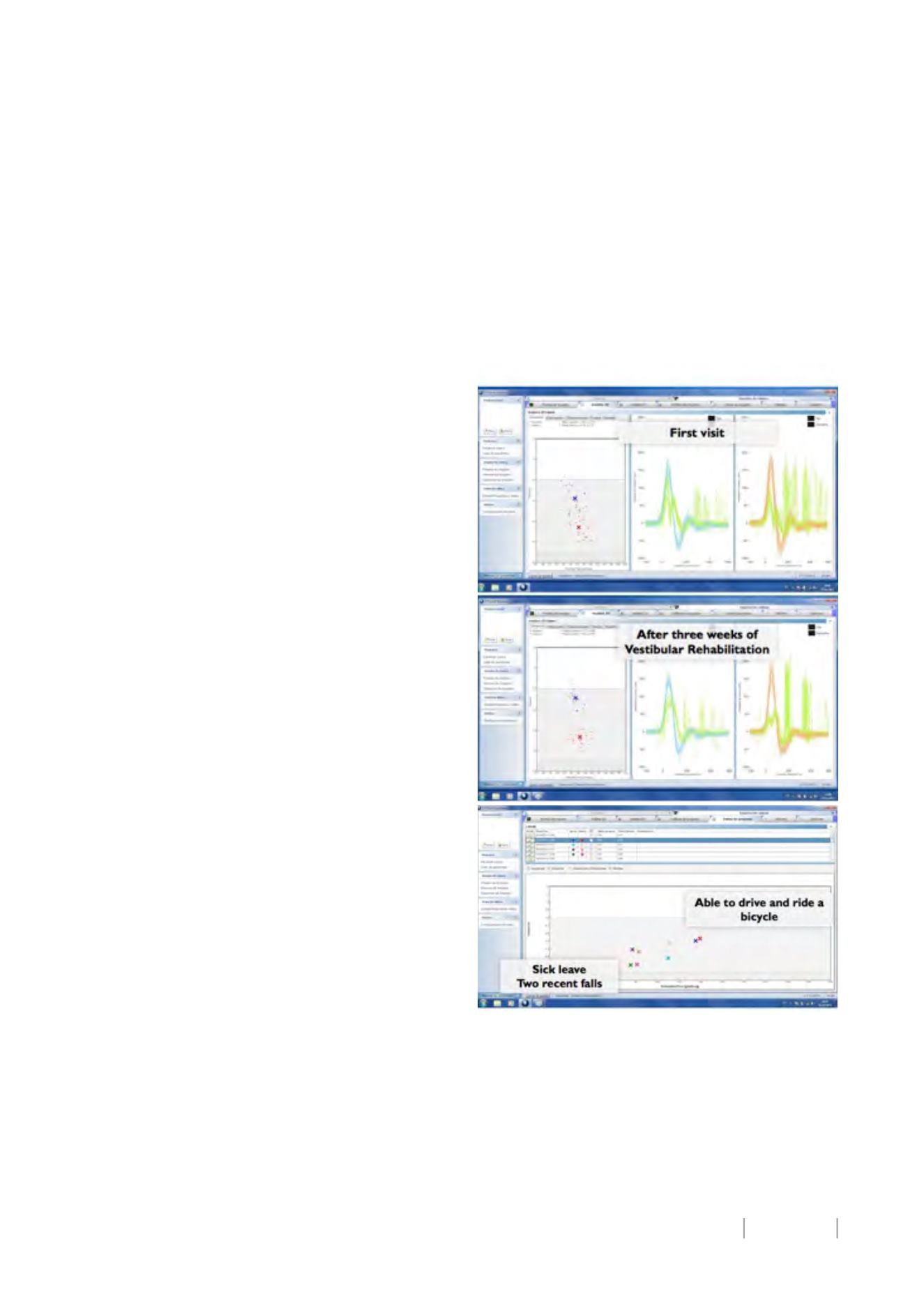
video hit impulse test, we demonstrate in figure 4 two different
possibilities. Inoneside, changeof thesaccadespatternshow the
evolution of treatment (without VOR gainmodification), and in
theother, recoveryof VORgain canbemeasuredeasily.
Figure 4. Effect of Rehabilitation and function recovery on
VHIT results. These are two different patients. On the right of the
figure, resultsbeforeandafter threeweeksof treatmentareshown
(change on the saccades pattern, without modification of VOR’s
gain).On the left, recoveryofVORalong follow-up.
5.- Posturography.-
is amethodof quantifying balance that
compares the results of Romberg test over different situations
(progressively more difficult, and removing or disrupting
sequentially visual, proprioceptive or both inputs). Classical
studies have assessed results of BVH patients with this test28,